Short Communication - Neuropsychiatry (2018) Volume 8, Issue 1
Psychiatric Symptoms and Electroencephalograms in Anti-NMDAR Encephalitis
- *Corresponding Author:
- Hiroshi Kataoka
Department of Neurology
Nara Medical University840 Shijo-cho, Kashihara, Nara 634-8522, Japan
Phone: +81-744-29-8860
Fax: +81-744-24-6065
Abstract
The awareness of anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis has been increasing throughout the world. Typically, psychiatric symptoms (PS) initially occur, followed by the development of seizures, involuntary movements, autonomic instability, or central hypoventilation.
Keywords
Anti-NMDAR Encephalitis, Epileptic seizures, Cognitive disorders, Memory disorders, Central hypoventilation
Discussion
When symptoms of anti-NMDA receptor encephalitis are classified into 8 categories of behavior cognitive disorders, memory disorders, speech disorders, epileptic seizures, dyskinesia, consciousness disorders, autonomic nervous symptom, and central hypoventilation, within 1 month of onset 87% of patients present with symptoms of more than 4 categories [1]. During the initial psychiatric presentations, neurological involvement such as memory problems is often minor. If a patient has only PS, the diagnosis can be delayed. The diagnosis is sometimes difficult because brain magnetic resonance imaging in most patients shows normal findings or nonspecific lesions, especially when other types of neurological involvement, such as oropharyngeal dyskinesia, are absent. Electroencephalography (EEG) shows some abnormalities, such as background slowing, even when only PS was evident [2,3]. I focus on PS in this disorder and electroencephalographic (EEG) findings during psychiatric presentations.
Typically, patients with anti-NMDAR encephalitis initially present with PS, followed by the development of florid neurological deterioration. Two-thirds of patients with NMDAR antibody encephalitis have prominent PS [4]. During the initial psychiatric presentations, mild neurological abnormalities such as orofacial dyskinesias and memory problems are often observed [5]. PS include various combinations of symptoms, such as delusions, delusional thinking, auditory or visual hallucinations, paranoid thoughts, aggression, irritability, confusion, bizarre behavior, paranoid thoughts, mania, anxiety, insomnia, or depressed mood. Non-specific commoncold- like prodrome (subfebrile temperature, headache, fatigue) precedes the psychiatric presentations. PS rarely persists without neurological involvement, and this prevalence is 4% [5]. Among 23 patients with the isolated PS, 74% patients had delusional thinking, 43% had auditory or visual hallucinations, 57% showed aggressive behavior, and 70% had a documented mood component [5]. A case report showed that PS without neurological involvement can persist for 14 years [6]. PS with or without mild neurological presentations do not necessarily progress to severer multisymptom disease, even if the period without treatment is prolonged [5]. Psychiatrists have reported that anterograde amnesia independently of PS or alteration of the perception of time is particularly evident in anti-NMDA receptor encephalitis [7]. For example, it sounds as if a song is being played in the reverse direction, or one day feels like 48 hours, and the surrounding people appear to be moving in slow motion. The author mentions that these symptoms are likely not to be evident in patients with schizophrenia. Psychological studies in healthy volunteers who received ketamine, which decreases the function of NMDA receptors, showed alteration of the perception of time [8]. Moreover, transient and sudden emotional changes that were not derived from personal experience occurred within several minutes to several periods of ten minutes [7]. For example, the patient was in a good mood and suddenly said “I want to die” and cried. PS often become prominent, and sedative medication is required for their management [5,9,10]. Eightythree percent of patients with isolated psychiatric episodes of anti-NMDAR encephalitis had good outcomes in response to immunotherapy and tumor removal [5].
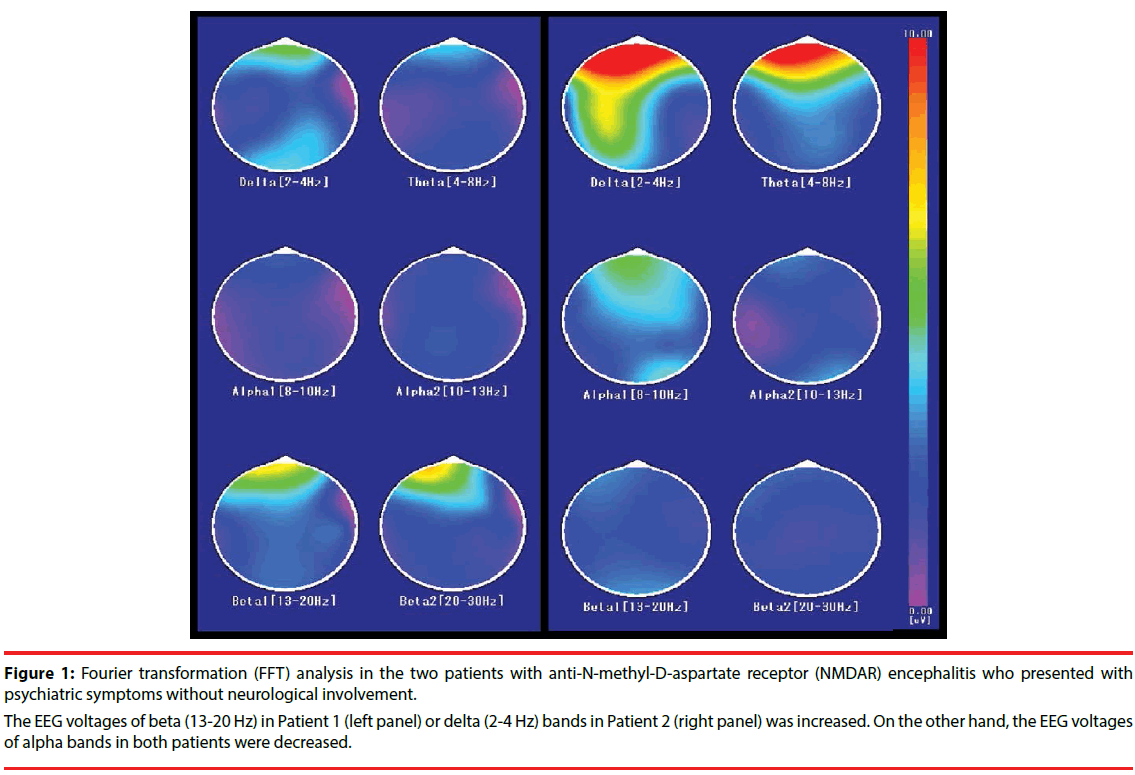
In acute encephalitis, the most frequent EEG finding is the presence of diffuse slowing of background activity [11]. In patients with anti- NMDAR encephalitis, diffuse background slowing or focal slow waves on EEG are usually seen, especially in the frontotemporal regions. Epileptic seizures were reported in 76% of adults [4] and 77% of children [4,12], and epileptic characteristics are not always evident during the initial psychiatric presentations. Extreme delta brush is a wave peak of 1-3 Hz delta waves superimposed on a large amount of 20-30 Hz beta waves. Extreme delta brush is a specific EEG finding in this disorder, but the sensitivity of 30% of the patients is low relative to the specificity [13]. Extreme delta brush is not present from the onset of disease, and indicates a more severe disease course, a prolonged disease course, or poorer outcomes at discharge [2,13]. The EEG abnormalities in anti-NMDA receptor encephalitis resolve along with clinical improvement [14]. In a previous study, 4 of 10 patients showed diffuse slowing and 1 patient showed focal slowing within 14 days of the first presentation of anti-NMDAR encephalitis [10]. Epileptic forms or extreme delta brush was seen in 2 patients and 1 patient, respectively. EEG was normal in 2 patients. One study performed by means of Fast Fourier transformation (FFT) analysis in 10 patients with anti-NMDAR encephalitis showed that beta activity was increased relative to delta activity in contrast to patients with other types of encephalitis [3]. This finding was observed at the earliest phase of the disease, especially in 4 patients in whom EEG was performed at the time of presenting with only PS. The 4 patients had diffuse slowing without an epileptic form. The authors suggested that the evidence of the increased beta activity as compared with delta activity might be a useful marker for the differential diagnosis of this encephalitis from other types of encephalitis. These patients did not have extreme delta brush. Another study of 16 patients, including 4 patients who presented with only behavioral changes and PS without neurological involvement, reported general delta activity in 7 patients, focal delta activity in 7 patients, and increased beta activity in 8 patients [2]. Low-voltage EEG activity associated with lower levels of consciousness during the acute phase predicts unfavorable neurological outcomes in acute encephalitis [15]. In a patient with anti-NMDAR encephalitis who presented with the initial PS, EEG voltages of alpha bands were decreased in all brain areas as compared with those of the healthy controls [16]. In our two patients in whom EEGs were performed at the initial PS (Table 1) [17,18], FFT analysis with the use of a frequency analyzer as described previously [16] showed increased voltage of beta activity or delta activity (Figure 1). During the initial psychiatric presentations, some alterations of EEG including delta or beta activity, lowvoltage EEG activity, or background slowing are often seen.
| Patient 1 [20] | Patient 2 [18] | |
|---|---|---|
| Age/sex at admission | 40 / M | 18 / M |
| psychiatric symptoms | delusions, delusional thinking, hallucinations, aggression, irritability, confusion, bizarre behavior, paranoid thoughts, manic | delusions, delusional thinking, paranoid thoughts, hallucinations, aggression, irritability, confusion, bizarre behavior, cataplexy, |
| prodominal symptoms | fatigue | subfebrile temperature, headache |
| followed neurological features | seizure** | Kluver Bucy syndrome |
| duration from phychiatric symptoms to first neurological feature [days] | 12 | - |
| WBC in CSF [/mm3] | 1 | 100 |
| first MRI abnormality | - | - |
| Treatments and outcomes | ||
| immuno-treatments | ST, IVIG | ST |
| surgery | - | - |
| Duration follow-up [months] | 72 | 3 |
| Outcome | under medications | complete recovery |
| EEG examination during psychotic stage | ||
| interval from EEG to neurological onset [days] | 6 | - |
| sedative drugs※ | low dose midazolam | low dose midazolam |
| anticonvulsant drugs※ | - | - |
| background diffuse slowing | + | - |
| epileptoform discharge | - | - |
| extreme delta blush | - | - |
| periodic complexities | - | - |
| WBC: white blood cells, CSF: cerebrospinal fluid, MRI: magnetic resonance imaging, EEG: electroencephalogram | ||
| ST: steroids, IVIG: intravenous immunoglobulin, ※during EEG examination | ||
| **: short periods and one attack of tonic seizures 12 days after the initial psychiatric presentation, and partial seizures were evident 6 year later. | ||
Table 1: Characteristics of two patients with anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis who presented with psychiatric symptoms without neurological involvement, and their EEGs were performed during the psychiatric symptoms.
Figure 1: Fourier transformation (FFT) analysis in the two patients with anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis who presented with psychiatric symptoms without neurological involvement.
The EEG voltages of beta (13-20 Hz) in Patient 1 (left panel) or delta (2-4 Hz) bands in Patient 2 (right panel) was increased. On the other hand, the EEG voltages of alpha bands in both patients were decreased.
Conclusion
The reported prevalence of seropositive anti- NMDAR antibodies in psychiatric patients is 12 of 121 patients with schizophrenia (9.8%), 2 of 70 patients with major depression (2.8%), and none of 38 patients with borderline personality disorder [19]. Other studies detected the presence of anti-NMDAR antibodies in serum in 3 of 46 patients with first-onset schizophrenia (6%) [20] and in none of 80 patients who met the DSM-IV-TR criteria for schizophreniaspectrum illness [21]. Patients with a history of psychosis associated with bipolar disorder or schizophrenia tend to display persistent EEG abnormalities even when not actively psychotic [22]. These facts should be kept in mind. During the initial psychiatric presentations, the presence of neurological involvement, such as involuntary movement or seizures, is useful for diagnosis. A prodome of fever or headache is also helpful for diagnosis. If the psychiatric presentations are confirmed to be caused by anti-NMDA receptor antibodies, the psychiatric symptoms are treatable.
Acknowledgement
We are extremely grateful to Professor Josep Dalmau (University of Pennsylvania, Philadelphia; and Institució Catalana de Recerca i Estudis Avançats (ICREA) (JD), Barcelona, Spain) and Professor Keiko Tanaka (Kanazawa Medical University, Kanazawa, Japan) for measuring the anti-N-methyl-D-aspartate receptor (anti-NMDAR) antibodies.
Disclosure
The authors report no conflicts of interest related with our paper.
Funding Statement
H.K received JSPS KAKENHI Grant Number (15K9356).
References
- Titulaer MJ, McCracken L, Gabilondo I, et al. Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet. Neurol 12(2), 157-165 (2013).
- Veciana M, Becerra JL, Fossas P, et al. EEG extreme delta brush: An ictal pattern in patients with anti-NMDA receptor encephalitis. Epilepsy. Behav 49(1), 280-285 (2015).
- Foff EP, Taplinger D, Suski J, et al. EEG Findings May Serve as a Potential Biomarker for Anti-NMDA Receptor Encephalitis. Clin. EEG. Neurosci 48(1), 48-53 (2017).
- Dalmau J, Gleichman AJ, Hughes EG, et al. Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet. Neurol 7(12), 1091-1098 (2008).
- Kayser MS, Titulaer MJ, Gresa-Arribas N, et al. Frequency and characteristics of isolated psychiatric episodes in anti–N-methyl-d-aspartate receptor encephalitis. JAMA. Neurol 70(9), 1133-1139 (2013).
- Heekin RD, Catalano MC, Frontera AT, et al. Anti-NMDA Receptor Encephalitis in a Patient with Previous Psychosis and Neurological Abnormalities: A Diagnostic Challenge. Case. Rep. Psychiatry 253891 (2105).
- Funayama M, Kato G, Mimura M. Differentiation of anti-NMDA receptor encephalitis from mental disorders. Rinshoshinkeishinri 24(1), 5-10 (2013).
- Pomarol-Clotet E, Honey GD, Murray GK, et al. Psychological effects of ketamine in healthy volunteers. Phenomenological study. Br. J. Psychiatry 189(1), 173-179 (2006).
- Tsutsui K, Kanbayashi T, Tanaka K, et al. Anti-NMDA-receptor antibody detected in encephalitis, schizophrenia, and narcolepsy with psychotic features. BMC. Psychiatry 12(1), 37 (2012).
- Zhang Y, Liu G, Jiang MD, et al. Analysis of electroencephalogram characteristics of anti-NMDA receptor encephalitis patients in China. Clin. Neurophysiol 128(7), 1227-1233 (2017).
- llis LS, Taylor FM. The electroencephalogram in herpes-simplex encephalitis. Lancet 1(7753), 718-721 (1972).
- Florance NR, Davis RL, Lam C, et al. Anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis in children and adolescents. Ann. Neurol 66(1), 11-18 (2009).
- Schmitt SE, Pargeon K, Frechette ES, et al. Extreme delta brush: a unique EEG pattern in adults with anti-NMDA receptor encephalitis. Neurology 79(11), 1094-1100 (2012).
- Nosadini M, Boniver C, Zuliani L, et al. Longitudinal electroencephalographic (EEG) findings in pediatric anti-N-methyl-D-aspartate (anti-NMDA) receptor encephalitis: the Padua experience. J. Child. Neurol 30(2), 238-245 (2015).
- Hosoya M, Ushiku H, Arakawa H, et al. Low-voltage activity in EEG during acute phase of encephalitis predicts unfavorable neurological outcome. Brain. Dev 24(3), 161-165 (2002).
- Kataoka H, Takatani T, Ueno S. Low-voltage EEG activity presenting from psychotic stage in a patient with anti-NMDA receptor encephalitis. BMJ. Case. Rep (2012).
- Kataoka H, Sawa N, Tonomura Y, et al. Early progression of brain atrophy in patients with anti-N-methyl-D-aspartate receptor encephalitis: Case reports. Medicine (Baltimore) 96(17), e6776 (2017).
- Matuoka K, Ashino H, Eura N, et al. A man with anti-N-methyl-D-aspartate (anti-NMDA) receptor encephalitis who relapsed in a short period. Seishinigaku 55(6), 561-564 (2013).
- Steiner J, Walter M, Glanz W, et al. Increased prevalence of diverse N-methyl-D-aspartate glutamate receptor antibodies in patients with an initial diagnosis of schizophrenia: specific relevance of IgG NR1a antibodies for distinction from N-methyl-D-aspartate glutamate receptor encephalitis. JAMA. Psychiatry 70(3), 271-278 (2013).
- Zandi MS, Irani SR, Lang B, et al. Disease-relevant autoantibodies in first episode schizophrenia. J. Neurol 258(4), 686-688 (2011).
- Masdeu JC, González-Pinto A, Matute C, et al. Serum IgG antibodies against the NR1 subunit of the NMDA receptor not detected in schizophrenia. Am. J. Psychiatry 169(10), 1120-1121 (2012).
- Narayanan B, O'Neil K, Berwise C, et al. Resting state electroencephalogram oscillatory abnormalities in schizophrenia and psychotic bipolar patients and their relatives from the bipolar and schizophrenia network on intermediate phenotypes study. Biol. Psychiatry 76(6), 456-465 (2014).