Case Report - Neuropsychiatry (2017) Volume 7, Issue 6
Klüver–Bucy Syndrome Induced by Bilateral Basal Ganglion Lesion
- Corresponding Author:
- Hsing-Cheng Liu
Department of Psychiatry Taipei City Psychiatric Centre
Taipei City Hospital, Taipei, Taiwan
Tel: 02-27263141; Ext: 1342
Abstract
Previous literature showed several etiologies result in Klüver-Bucy syndrome. The most common involved region is the bilateral mesial temporal lobes. In this article, we present the first case of Klüver-Bucy syndrome that occurred after CNS infection with bilateral basal ganglion lesion, which linked the sensory, motor and reward information by cortico-basal ganglia circuitry.
Keywords
Kluver-Bucy syndrome, Basal ganglion, Infection, Cortico-basal ganglia circuitry, Temporal lobe
Introduction
Klüver–Bucy syndrome is a rare neuropsychiatric disorder and consists of placidity, docility, visual agnosia, dietary changes, hypersexuality and hyperorality which initially observed in a rhesus monkey after bilateral temporal lobotomy. Many etiologies have been reported in human; include CNS infection, cerebrovascular events, tumors, and various neurodegenerative disorders. The most common involved region is the bilateral mesial temporal lobes [1]. In this article, we present the first case of Klüver–Bucy syndrome in the world that occurred after CNS infection with bilateral basal ganglion lesion.
Case Report
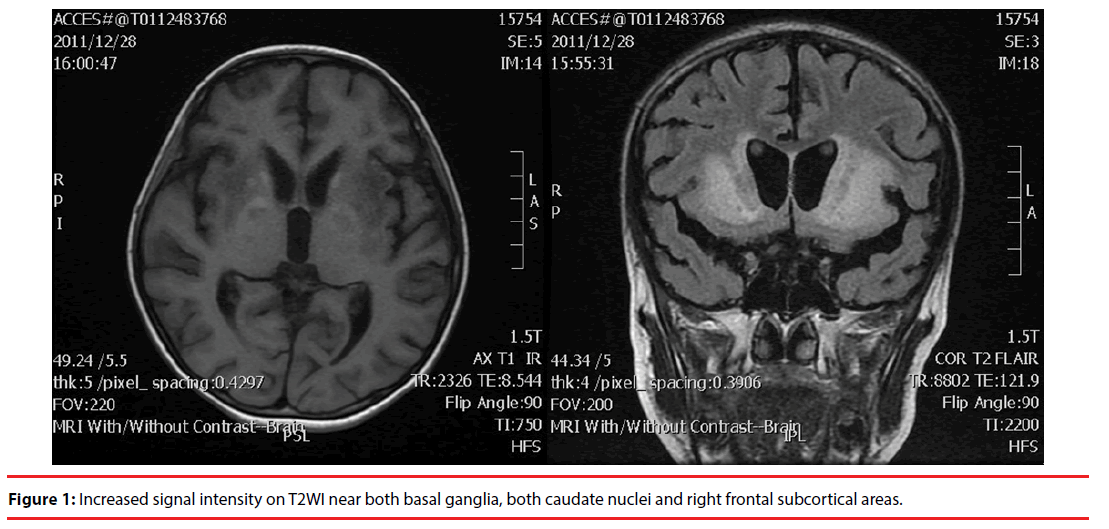
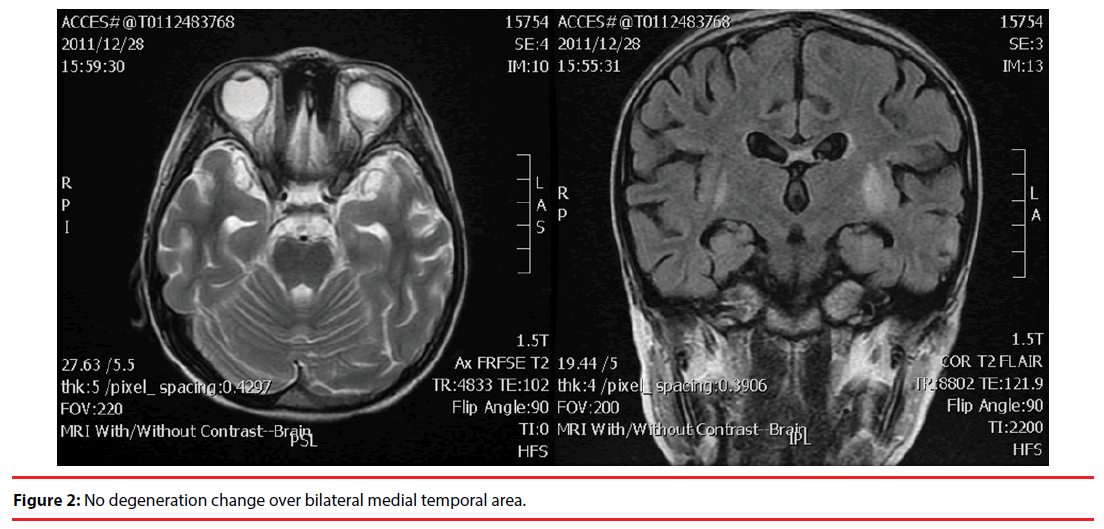
This 11-year-old boy was admitted to acute psychiatric ward due to his disrupted behavioral and emotional symptoms, which presented for nearly two years after CNS infection. Tracing back his history, he contracted an acute CNS infection with presentation of fever, generalized tonic-clonic seizure and conscious disturbance at the age of nine. The infection pathogen was proved to be mycoplasma by serological testing of the presence of mycoplasma IgM. After antibiotics, anticonvulsant and supportive care, he survived with general weakness and aphasia at first. He gradually recovered from the weakness and responsiveness also improved. However, he started to have various abnormal behaviors progressively six months later. The aberrant behaviors included hyperorality (tendency to touch objects by mouth and kiss others), hypermetamorphosis (strong tendency to react to visual stimulus), dietary changes (eat stool), loss of previously existing fears (increased aggressive behavior), and hypersexuality (masturbate in public). At school, he can’t focus on lectures. The annoying behavior included increasing attentiveness to visual stimuli around him and a need to touch most of the things entered his sight. He frequently kissed other female classmates and used the dirty words towards young lady teacher. Brain MRI revealed lesion over bilateral basal ganglion (Figure 1) and no positive finding over medial temporal area (Figure 2).
When we saw the patient at the age of 11, he still had above aggressive and impulsive behavior. The intellectual functioning test was done which showed full-scale IQ score was 67, what placed him below average. We treated him with risperidone 2mg/d and valproate 600mg/d; however, the effects were limited.
Discussion
This case meets the criteria of Klüver– Bucy syndrome: which includes changes in dietary habits, excessive oral tendencies, hypermetamorphosis, placidity and altered sexual behavior.
The previous reports showed that the Klüver– Bucy syndrome mostly occur after bilateral temporal lobe damage. Extratemporal involvement can be seen in up to 20-30% of the cases [2-4]. The most affected extratemporal lesions are seen in the frontal and parietal cortices, the occipital lobe, and brain stem. Our patient showed his main lesion in bilateral basal ganglion with preservation of bilateral medial temporal structures. Compelling evidence suggests that basal ganglion is involved in mediating human behaviors via so-called cortico-basal ganglia circuitry, the cortices include prefrontal cortex, limbic, and sensorimotor cortex [5,6]. It plays an important role in linking the sensory, motor and reward information. The reward system mechanism may in charge of human motor control. If the cortico-basal ganglia circuitry disrupt, could contribute to a variety of emotional, motor and cognitive symptoms associated with psychiatric disorders [7].
Until now, there is no specific medication for Klüver–Bucy syndrome; several reports showed that the annoying behavior might respond to the treatment carbamazepine, risperidone and selective serotonin reuptake inhibitors (SSRIs). Some experts use in combination with clonidine, methylphenidate and lamotrigine [8,9]. Actually, the drug history of the patient demonstrated that he did respond to these medications.
Conclusion
In conclusion, the case of our patient suggested that bilateral basal ganglion might be an extratemporal lesion for Klüver–Bucy syndrome. The optimal treatment for this distressful condition needs further investigation.
References
- Auvichayapat N, Auvichayapat P, Watanatorn J, et al. Kluver–Bucy syndrome after mycoplasmal bronchitis. Epilepsy. Behav 8(1), 320-322 (2006).
- Wasay M, Mekan SF, Khelaeni B, et al. Extra temporal involvement in herpes simplex encephalitis. Eur. J. Neurol 12(6), 475-479 (2005).
- Jereb M, Lainscak M, Marin J, et al. Herpes simplex virus infection limited to the brainstem. Wien. Klin. Wochenschr 117(13-14), 495-499 (2005).
- Mondal G, Kumar R, Ghosh JK, et al. Basal ganglia involvement in a child with herpes simplex encephalitis. Indian. J. Pediatr 76(7), 749-750 (2009).
- Ikemoto S, Yang C, Tan A. Basal ganglia circuit loops, dopamine and motivation: A review and enquiry. Behav. Brain. Res 290(1), 17-31 (2015).
- Gyorfi O, Nagy H, Bokor M, et al. Behavioural aspects of a modified crosstalk between basal ganglia and limbic system in Parkinson’s disease. Neuropsychopharmacol. Hung 18(2), 087-092 (2016).
- Marchand WR. Cortico-basal ganglia circuitry: a review of key research and implications for functional connectivity studies of mood and anxiety disorders. Brain. Struct. Funct 215(2), 73-96 (2010).
- Cohen MJ, Park YD, Kim H, et al. Long-term neuropsychological follow-up of a child with Klüver–Bucy syndrome. Epilepsy. Behav 19(4), 643-646 (2010).
- Coşkun M, Alyanak B, Yapıcı Z. Kluver-Bucy and Frontal Syndromes Following Meningoencephalitis in a Young Boy: Pathophysiological and Clinical Considerations. Arch. Neuropsy 49(2), 163-166 (2012).