Research Article - (2018) Volume 8, Issue 6
Is the Psychogenic Factor an Exclusive Contributor to Erectile Dysfunction in a Man Under Thirty?
- *Corresponding Author:
- Geng-Long Hsu
Microsurgical Potency Reconstruction and Research Center, 3F 88, Wen-Hu Street Nei-Hu Dt. 114, Taipei, Taiwan
Tel : 886-2-87526087
Fax: 886-2-87975207
Abstract
Albeit penile veins are the principal components in erectile rigidity in cadaveric hemodynamic studies, clinically, psychogenic factors play an exclusive role in a young adult with erectile dysfunction (ED), additionally the placebo effect affecting approximately 40% of the participants in clinical trials. This study addresses whether psychogenic contributor has an exclusive role in ED in males under the age of 30. This article is a review of literature obtained using MEDLINE. The information obtained was assessed regarding erectile physiology and ED pathophysiology. Although phospho-di-esterase-5 inhibitors have become the most widely adopted ED medical treatment with gained acceptance in ED pathophysiology, a refined penile venous stripping procedure also holds merit. An apagogical hemodynamic study was conducted on defrosted cadavers based on an innovative understanding of the penile venous anatomy. In our extensive clinical experience with the penile venous stripping method, this procedure is a viable treatment option for ED in males younger than 30 years of age. Thus, penile veins themselves are the most crucial factors in erection physiology, and venogenic factors are inappropriately considered as cavernosal factors in the list of ED contributors. Penile veins play a pivotal role in erectile rigidity and consequently, venous dysfunction is prevalent in males with ED. However, the psychological contribution is still paramount, although not exclusive, roles in ED in males younger than 30 years of age.
Keywords
Erectile dysfunction, Erection rigidity, Penile erection-related veins, Psychotherapy, psychogenic
Abbreviations
CC: Corpora Cavernosa; CV: Cavernosal Vein; DA: Dorsal Artery, DDV: Deep Dorsal Vein, ED: Erectile Dysfunction; IIEF: International Index Of Erectile Function; PAV: Para-Arterial Vein; PDE-5: Phosphodiesterase Type 5; PVSS: Penile Venous Stripping Surgery; USPTO: The United States Patent and Trade Office; VOD: Veno-Occlusive Dysfunction
Introduction
Erectile function depends on the seamless interplay between healthy psychologic, endocrinologic, vascular and metabolic factors, as well as the adequate function of cavernosal sinusoids [1]. An erectile dysfunction (ED) will ensue if a sufficiently rigid penile erection for coitus cannot be satisfactorily attained or maintained [2]. ED has troubled the human race for generations and demands research in every society to uphold human rights [3].
Recent research enables us to understand how penile erection is achieved by uncovering the vital role of smooth muscle relaxation of the corpus cavernosum [4]. Additionally, a list of ED contributors has been established including psychogenic disturbance, endocrinologic disorders, arterial insufficiency, neurologic deficits, pharmacological adverse effects, metabolic syndrome or cavernosal disintegration [5]. Is the role of penile veins being inadvertently ignored from the erection physiology? Is the venogenic factor equivalent to the cavernosal factor as a contributor given that venous leakage plays a major role in ED males without comorbidity and in those whose ED is a consequence of cigarette smoking [6,7]?
Young males can achieve a rigid erection by imagination, fantasying, and visual or auditory stimulation, therefore psychogenic disturbance is generally considered to be the main cause of ED for males under the age of 40 according to the literature [8,9]. Males cannot enjoy sex without adequate mental function even when equipped with a functional penis. However, the previously believed purely psychogenic causes behind ED were replaced by majorly organic etiologies with the identification of veno-occlusive dysfunction in the phallo-dynamic era [10,11]. The dispute regarding the cause of ED might be over as the vasculogenic factors gains its volume of voice in the etiology of organic ED [12,13]. Between 1986 and 1987, we performed penile venous stripping surgery (PVSS) to five men under the age of 30 [14]. We were encouraged to know that their unassisted natural coitus was satisfactory (IIEF-5=19-24) even though two of them were later diagnosed with psychological problems [15].
In 2011 an international journalist team observed our PVSS procedure from the United Kingdom. We were asked why penile venous surgery is often condemned despite its acknowledgement as an ideal vascular surgery. To answer, penile vasculature is too delicate to be seen in detail and PVSS is a challenging procedure to observe. Therefore, urological surgeons will not recommend it since it is beyond the common “seeing is believing” rule. Nowadays, it is easier to appreciate how PVSS can be performed with the help of video recording equipment under adequate magnification. Importantly, though anatomically the penis is in the realms of urology, the delicate microsurgery is beyond the traditional urology training, which may result in an inadequate skill level leading to an unfavorable outcome. Together with our clinical experience on thousands of ED males in the past three decades and hundreds of cadaveric studies, we challenge the common belief that penile venous origin should be excluded as one of the major causes of ED. Furthermore, we argue that penile venous surgery, particularly PVSS, should not be abandoned. Dozens of young males from all over the world visited our PVSS clinic seeking a solution for their ED. Many of them posed concerns as to why their urologists always attributed their problem as caused by a psychogenic factor [16,17]. Most physicians reprimand these young ED patients by telling them “your ED is caused by your brain” or simply labels them as “too afraid to have intercourse,” On the contrary, we believe that ED in many young patients was mainly of venogenic origin since their problem improved dramatically by PVSS. The problem left is how to differentiate the venous origin from the psychogenic origin. In order to demonstrate that a psychologic factor has little influence in ED, we carried out a series of hemodynamic studies in both fresh and defrosted cadavers [18,19].
Methods
This article details the findings of our cadaveric hemodynamic study and is supplemented by a literature review. Journals in the fields of andrology, anatomy, epidemiology, internal medicine, neuropsychiatry, sexual medicine and urology were searched through MEDLINE in November 2016 for papers published from 1873 onwards. The search used the following terms in various combinations: erectile dysfunction, erection rigidity, penile erection-related veins, psychotherapy, and psychogenic. The literature search was reviewed by two authors and discrepancies were resolved. The information obtained was assessed for the topic involving erectile physiology, ED pathophysiology, ED causes, and contemporary management of ED.
Results
▪ Interplay of psychology and physiology in medicine, which is the protagonist?
The essential role of psychology. There is no way to enjoy a love life without a healthy working central nervous system. It is especially true for sexual activity because erection, emission, ejaculation and orgasm are specifically coordinated by corresponding areas in the brain [20-22]. Interestingly, it is also true for clitorial erection in the female counterpart [23]. An intact limbic system is essential to receive pleasure rewarding. The sensitivity of the glans penis requires brain interpretation. Without a functional brain, a penile erection becomes meaningless. The introduction of brain mapping benefits the research on erection issues [24-27].
Interplay of psychology and physiology their role together. Throughout medical history, clinicians have endeavored to identify contributors in each disease entity. Psychotherapy consistently plays a leading role in solving the most human problem because psychological factors always contribute to some extent [28,29]. The observation of the power of nothing, the placebo effect, has changed the way we think about medicine [30]. ED is no different; indeed, ED was previously thought to be entirely caused by a psychogenic factor. Although our current evidence does not support this notion, we cannot ignore its contribution. The importance of psychotherapy in ED treatment has not changed over time [31]. Can the power of a psychogenic role in ED be validated by the effectiveness of a placebo treatment? Some studies have suggested that children and adolescents are more prone to respond to a placebo than adults [32-34], a finding that is comparable to adult studies [35]. Chen et al. reported a randomized, double‐blind, parallel, placebo‐controlled clinical trial using oral tadalafil in the treatment of men with ED in 2004. It was interpreted that a psychological factor explained 42.8% of the ED issues in that study [36].
Billions of people suffer from ED. It was previously believed that ED requires a multiple disciplinary management. The introduction of sildenafil has changed the concept [37,38]. There is a belief that there is no longer a need for Collaboration between healthcare practitioners from different disciplines in term of the evaluation, treatment, and education issues surrounding sexual dysfunction with the high response rate to sildenafil. However, neither psychotherapy alone nor medical intervention alone is sufficient to resolve sexual problem [39]. ED requires an individualized and integrated management to achieve a lifelong solution.
▪ Role of sex therapy in erectile dysfunction
Sex therapy in ED. Sex therapy, a form of psychotherapy, has existed throughout human history in different cultures, including China, India, Egypt, Greece, and Rome [40,41]. Numerous forms have been used involving specific manuals; Yoga; meditation; spells; aphrodisiacs (deer antelope, tiger penis, herb and acupuncture, etc.) according to the literature[42,43]. Interestingly some of them might be helpful based on modern scientific research [44]. Obviously, there is merit to conduct further research on the efficacy of them for treatment of ED [45].
▪ Differentiating normal ED from psychological ED
There is no way to single out a psychogenic cause in ED and clinicians have to differentiate the psychogenic from organic contributors before ignition of management. Tremendous advancement in modern medicine has enabled physicians to identify ED contributors effectively. The factors that are helpful in differentiating normal erectile function from psychological ED include affecting indifference during sexual stimulation, sexual arousal indifferences, poor perception of control over arousal, distractibility during sexual stimulation, and difficulty in declining a sexual response while anxious [46,47]. Every ED clinician has experience in treating patient with a psychiatric disorder. Integrated assessment is the cornerstone for establishing the correct diagnosis, and sex therapy may be an indispensable part of a successful treatment for certain patients [48]. ED clinicians should adopt a multidisciplinary strategy that includes not only the collaboration with other professionals, but also integrates contemporary knowledge to provide a structured approach to personalized ED management [49].
▪ Innovative penile tunical and venous anatomy
▪ Discovery of Penile tunical and venous anatomy.
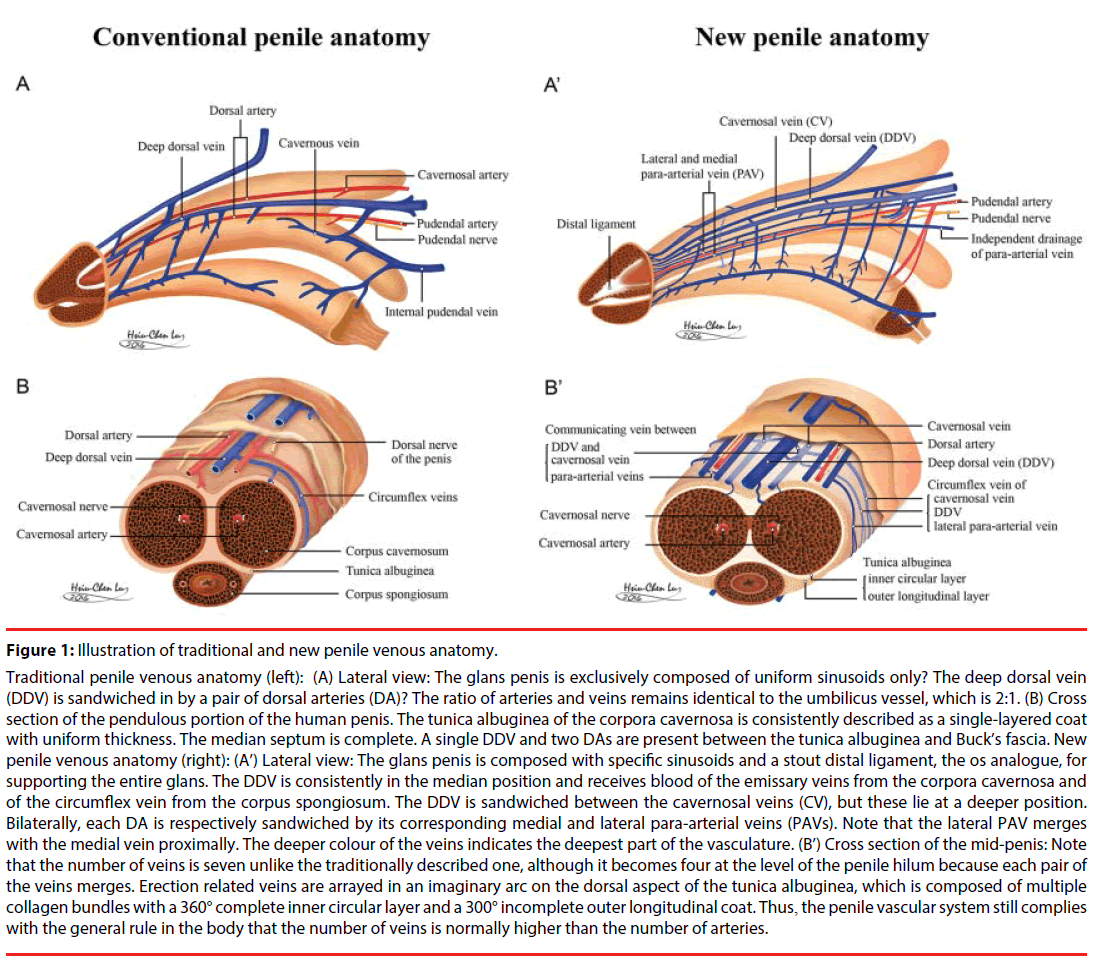
The human penis has been in its current anatomic form for 3000 centuries [50]. It is a unique structure composed of multiple fascial layers surrounding the three extensible cylinders with independent sinusoids, i. e. the glans penis, the corpus spongiosum and the paired corpora cavernosa (CC). The CC is encircled by the tunica albuginea which is composed of multiple collagen bundles and exclusively responsible for erectile rigidity. The penile tunical anatomy has been widely studied and is, however, consistently described as a single layer with uniform thickness and strength circumferentially the (Figure 1, left) [51]. Our study substantiates a model of the tunica albuginea of the corpora cavernosa as a bi-layered structure with a 360° complete inner circular layer and a 300° incomplete outer longitudinal coat (Figure 1, right) [52]. A rigid erection ensues only after a sound interplay is achieved by the tunica albuginea and penile erection related vasculature. As for the penile erection related vasculature, a single deep dorsal vein (DDV) is consistently depicted between the tunica albuginea and Buck’s fascia, and is flanked by a pair of the dorsal artery (Figure 1A,B). Should then the penile vasculature be an exception to the standards of the human body with the ratio of the number of arteries to veins as 1:2? Our extensive study over the past 3 decades has revolutionized the understanding of the erection related veins into (1) a DDV, (2) a pair of cavernosal veins (CV) and (3) two pairs of para-arterial veins (PAV) (Figure 1A, B) [53].
Figure 1: Illustration of traditional and new penile venous anatomy.
Traditional penile venous anatomy (left): (A) Lateral view: The glans penis is exclusively composed of uniform sinusoids only? The deep dorsal vein (DDV) is sandwiched in by a pair of dorsal arteries (DA)? The ratio of arteries and veins remains identical to the umbilicus vessel, which is 2:1. (B) Cross section of the pendulous portion of the human penis. The tunica albuginea of the corpora cavernosa is consistently described as a single-layered coat with uniform thickness. The median septum is complete. A single DDV and two DAs are present between the tunica albuginea and Buck’s fascia. New penile venous anatomy (right): (A’) Lateral view: The glans penis is composed with specific sinusoids and a stout distal ligament, the os analogue, for supporting the entire glans. The DDV is consistently in the median position and receives blood of the emissary veins from the corpora cavernosa and of the circumflex vein from the corpus spongiosum. The DDV is sandwiched between the cavernosal veins (CV), but these lie at a deeper position. Bilaterally, each DA is respectively sandwiched by its corresponding medial and lateral para-arterial veins (PAVs). Note that the lateral PAV merges with the medial vein proximally. The deeper colour of the veins indicates the deepest part of the vasculature. (B’) Cross section of the mid-penis: Note that the number of veins is seven unlike the traditionally described one, although it becomes four at the level of the penile hilum because each pair of the veins merges. Erection related veins are arrayed in an imaginary arc on the dorsal aspect of the tunica albuginea, which is composed of multiple collagen bundles with a 360° complete inner circular layer and a 300° incomplete outer longitudinal coat. Thus, the penile vascular system still complies with the general rule in the body that the number of veins is normally higher than the number of arteries.
▪ Comparative penile anatomy
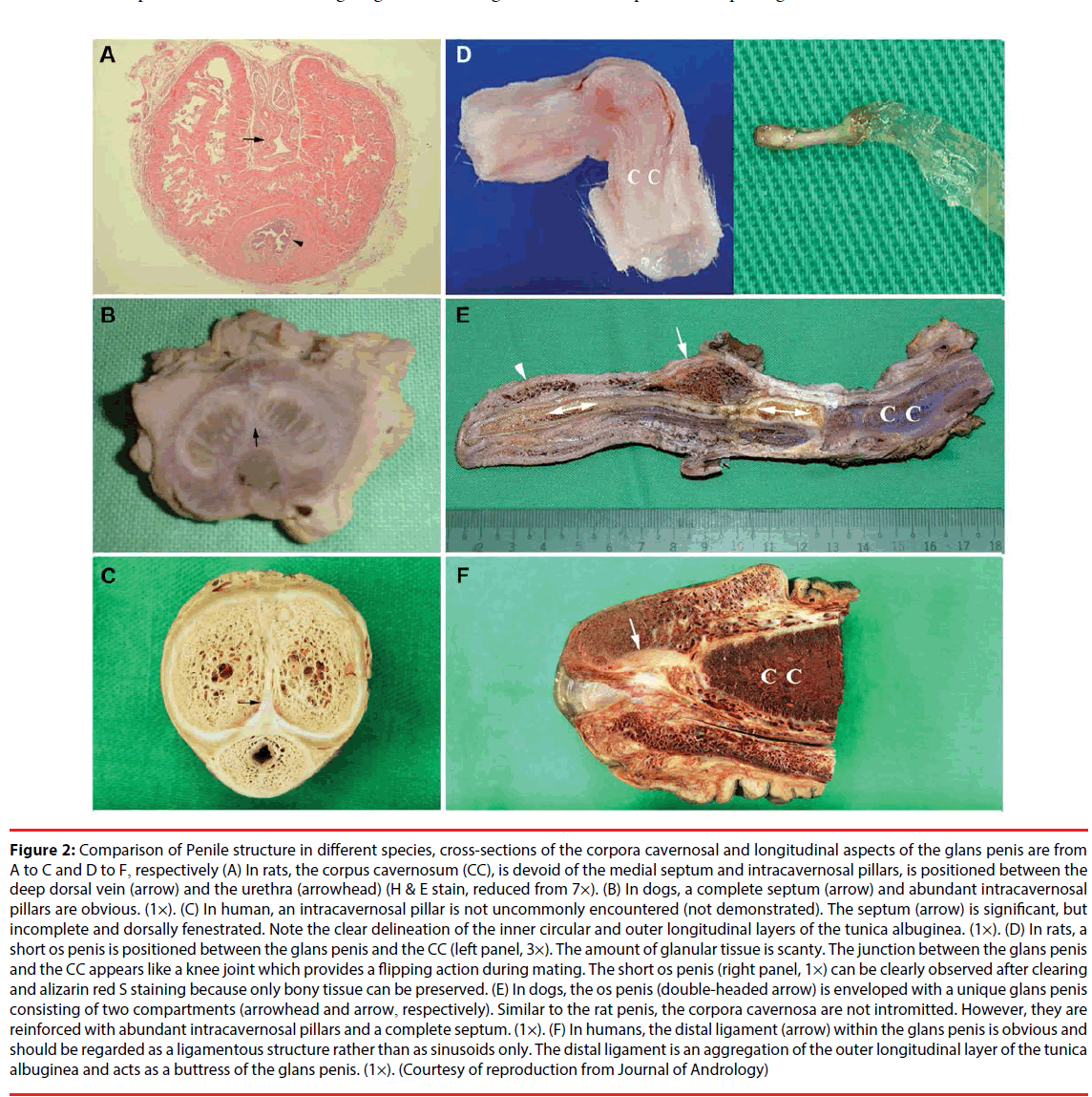
Both penile tunical and venous anatomy were not discovered until our endeavor in recent studies including penile tunical anatomy, penile venous anatomy and a comparative penile anatomy in varied species [54]. The tunical outer layer originates from the bulbospongiosus and ischiocavernosus proximally and extends continuously into the distal ligament, os analogue, within the glans penis [55,56]. This layer is the determining structure responsible for the penile shape and penile implant protection. Therefore, it is extremely crucial in penile morphology reconstruction and penile implantation [57,58]. The os penis exists in mammalian species, such as the dog and rat, for providing eternal rigidity. Although the os penis is traditionally believed to be absent in human, an os analogue does exist instead (Figure 2). How can the human glans penis bear the buckling pressure generated from coitus without the os analogue? Furthermore, the anatomical location and histology of the distal ligament invite convincing parallels with the quadruped os penis; therefore, it constitutes the potential evidence of the evolutionary process. In summary, the CC, a chamber design by Mother Nature, is responsible for facilitating rigid erections. For investigating venogenic factors, hemodynamic studies have been conducted on both fresh and defrosted human male cadavers. In each case, a rigid erection was unequivocally attainable following the removal of erection related veins. This clearly has a significant impact on penile venous surgery and has a vital role in treating impotent patients. The newly identified information about penile tunical, venous anatomy and erection physiology was inspired by, and in turn, enhance clinical applications by physicians and surgeons, such as penile morphological reconstruction, penile implantation, and PVSS [59-62]. Additionally, the above information helps us to answer questions frequently raised during patient counsellings.
Figure 2: Comparison of Penile structure in different species, cross-sections of the corpora cavernosal and longitudinal aspects of the glans penis are from A to C and D to F, respectively (A) In rats, the corpus cavernosum (CC), is devoid of the medial septum and intracavernosal pillars, is positioned between the deep dorsal vein (arrow) and the urethra (arrowhead) (H & E stain, reduced from 7×). (B) In dogs, a complete septum (arrow) and abundant intracavernosal pillars are obvious. (1×). (C) In human, an intracavernosal pillar is not uncommonly encountered (not demonstrated). The septum (arrow) is significant, but incomplete and dorsally fenestrated. Note the clear delineation of the inner circular and outer longitudinal layers of the tunica albuginea. (1×). (D) In rats, a short os penis is positioned between the glans penis and the CC (left panel, 3×). The amount of glanular tissue is scanty. The junction between the glans penis and the CC appears like a knee joint which provides a flipping action during mating. The short os penis (right panel, 1×) can be clearly observed after clearing and alizarin red S staining because only bony tissue can be preserved. (E) In dogs, the os penis (double-headed arrow) is enveloped with a unique glans penis consisting of two compartments (arrowhead and arrow, respectively). Similar to the rat penis, the corpora cavernosa are not intromitted. However, they are reinforced with abundant intracavernosal pillars and a complete septum. (1×). (F) In humans, the distal ligament (arrow) within the glans penis is obvious and should be regarded as a ligamentous structure rather than as sinusoids only. The distal ligament is an aggregation of the outer longitudinal layer of the tunica albuginea and acts as a buttress of the glans penis. (1×). (Courtesy of reproduction from Journal of Andrology)
▪ Hemodynamic experiments on human cadavers: the power of Reductio ad absurdum
▪ Human erectile physiology
The human erectile mechanism is an intricate balance between hormonal, vascular, neurological, sinusoidal, pharmacological, and psychological factors. However, the mechanism itself and the relative contribution of each respective component remain somewhat unclear, and merit further study. To identify a research model for differencing venogenic factors from psychogenic factors in the ED contributor list, cadavers were deliberately chosen. A dynamic cavernosometry was performed in 48 cadavers for various hemodynamic studies (Table 1). From 2002-2003, five fresh cadavers were obtained for demonstrating the pivotal role of the penile erection related veins in a penile erection [18]. It was criticized that our model used normal saline with a speed of 150 mL/min which far exceeds the arterial inflow rate of 60-80 mL/Min in human penile physiology. A second criticism regarded how to prove the sinusoidal cells were totally dead. Although normal saline is used for volume expansion in medical purposes, the viscosity coefficient is zero, and subsequently, the infusion rate will be abnormally high. We then use 10% colloid and defrosted cadavers for nullifying the two concerns.
| Grouping | Cadaver | Infusion rate or volume | Purpose of study for penile erection-related veins* [Reference] |
|||
|---|---|---|---|---|---|---|
| No. | Study time | Fluid | Preoperative † | Postoperative | ||
| Fresh | 5 | 2002-2003 | Normal saline | 1050 mL | 89 mL | the pivotal role in erection [18] |
| Defrosted Defrosted Defrosted |
15 7 11 |
2009-2010 2010-2012 2011-2013 |
10% colloid 10% colloid 10% colloid |
28.1 mL/min 30.2mL/min |
7.3mL/min 2.8mL/min |
the principal component in erectile rigidity [19] venous drainage of the corpora cavernosa [63] role in penile veno-occlusive Mechanism [64] |
| Total | 48 | |||||
* Penile erection-related veins (PERV) include one deep dorsal vein, two cavernosal veins and two and pairs of para-arterial veins
†The PERV stripping surgery.
Table 1: Summary of hemodynamic study on 48 valid human male cadavers in varied purposes from 2002 to 2013.
▪ Simulating hemodynamic physiology in the human penis
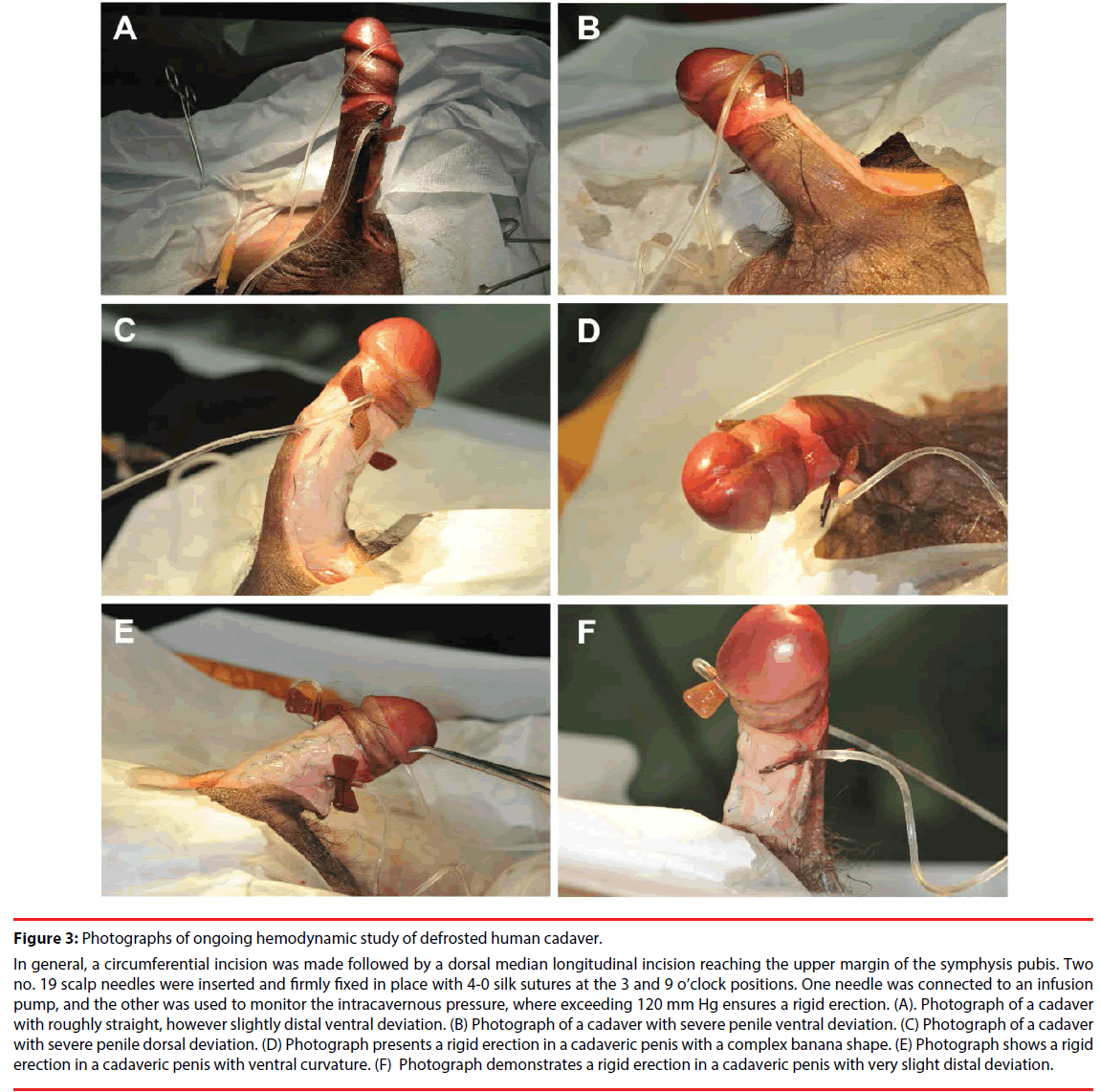
We investigated the role of venous outflow in an attempt to isolate the key determinant of erectile function. The dynamic infusion cavernosometry and cavernosography were conducted on 15 defrosted human cadavers (Figure 3), both before and after the meticulous removal and ligation of penile veins. Preoperatively, an infusion rate of more than 28.1 mL/min (14.0 - 85.0 mL/min) was required to induce a rigid erection. Following surgery, we obtained the same result at a rate of 7.3 mL/ min (3.1 - 13.5 mL/min) across the entire sample. The rigid erection is a mechanical phenomenon, and penile veins are the principal component for erectile rigidity [19]. Similarly, 7 cadavers were studied for exploring the venous drainage of the CC [63]. Eventually, 11 valid defrosted cadavers were studied via electrocautery (n=6) or ligation (n=5) and indirectly proved the venous occlusion mechanism (n=11) [64]. Given the fact that we eliminated the influence of hormonal, arterial, neurological, sinusoidal, pharmacological, and psychological factors while the sinusoidal tissue was not viably extensible in cadavers, we believe that our study clearly demonstrated that the human erection is fundamentally a mechanical event contingent on venous competence. Did the results from the hemodynamic study confirm our hypothesis by the power of Reductio ad absurdum? We challenged the general belief that the venogenic factors is considered equivalent to cavernosal factors in the list of ED contributor [5].
Figure 3: Photographs of ongoing hemodynamic study of defrosted human cadaver.
In general, a circumferential incision was made followed by a dorsal median longitudinal incision reaching the upper margin of the symphysis pubis. Two no. 19 scalp needles were inserted and firmly fixed in place with 4-0 silk sutures at the 3 and 9 o’clock positions. One needle was connected to an infusion pump, and the other was used to monitor the intracavernous pressure, where exceeding 120 mm Hg ensures a rigid erection. (A). Photograph of a cadaver with roughly straight, however slightly distal ventral deviation. (B) Photograph of a cadaver with severe penile ventral deviation. (C) Photograph of a cadaver with severe penile dorsal deviation. (D) Photograph presents a rigid erection in a cadaveric penis with a complex banana shape. (E) Photograph shows a rigid erection in a cadaveric penis with ventral curvature. (F) Photograph demonstrates a rigid erection in a cadaveric penis with very slight distal deviation.
▪ Penile venous stripping for treatment of erectile dysfunction
▪ Conventional penile venous surgery
In 1873, Parona proposed that varicosity could lead to penile dorsal vein dysfunction [65]. In 1902, Wooten proposed deep penile vein ligation as the cure for atonic impotence [66]. Although Lowsley and Rueda performed this procedure multiple times in their 1953 report [67], similar procedures were not popular for restoring erectile function until 1985 [68]. However, this popularity dwindled away over time [69]. We agreed that this procedure should be abandoned because of its disappointing outcomes with seemingly unavoidable complications such as irreversible deformity and permanent penile numbness [70].
▪ Anatomy-based penile venous stripping for treating ED.
Despite these drawbacks, our PVSS procedure, a well-designed modification of the conventional venous surgery, has been developed after numerous positive responses from our patients. Since 1986, our success was built upon our better understanding of penile tunical and venous anatomy associated with the erection mechanism [15,53,64]. We continuously refined the PVSS technique through a large patient population under acupuncture-assisted local anaesthesia performed in a one-day surgery clinic. We have been contacted by patients all over the world seeking the procedure after their poor functional outcomes and unexpected adverse effects from prior penile vascular intervention [71]. As a matter of fact, the conventional penile venous surgery has been officially rejected by the European Urological Association [72].
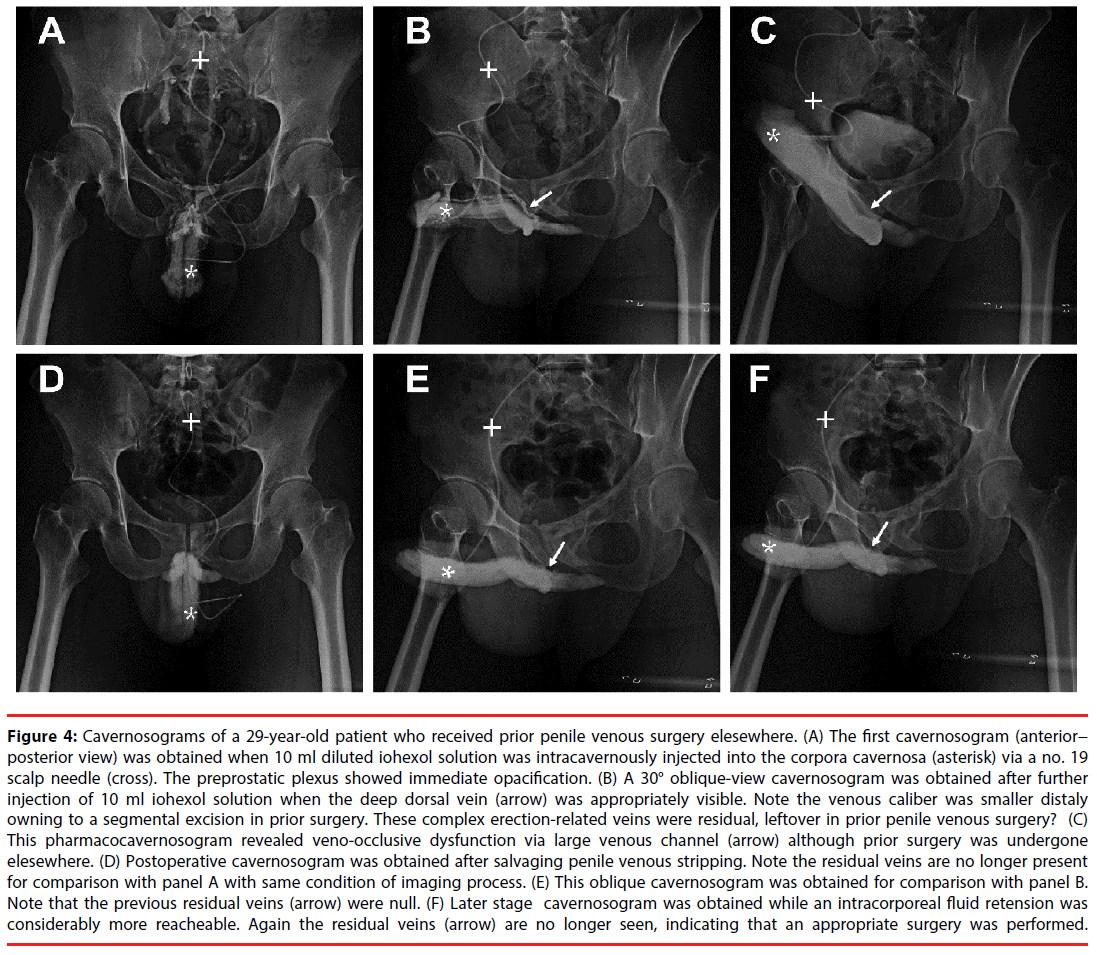
▪ Two main causes for unsuccessful conventional penile venous surgery
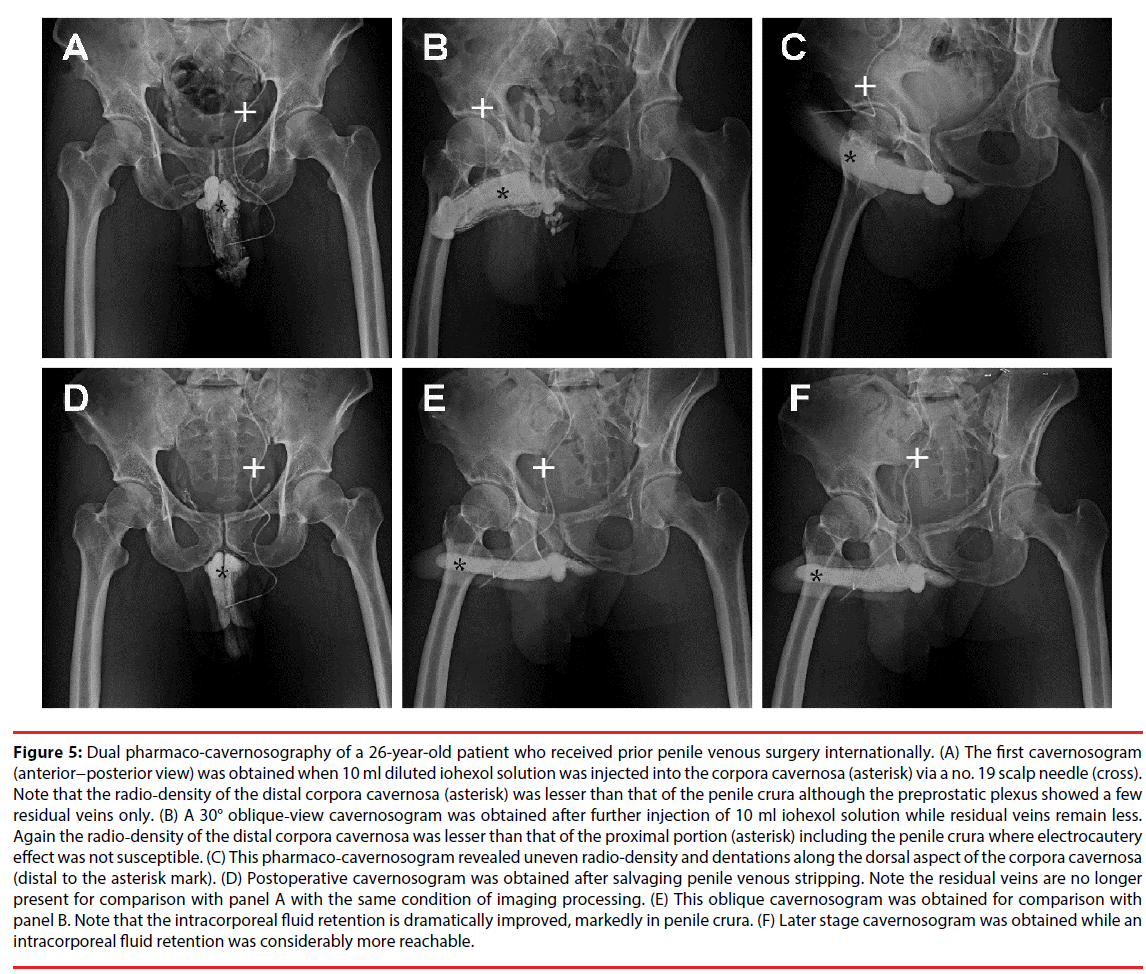
Although currently, we recommend PVSS only to patients who failed to response to phosphodiesterase-5 (PDE-5) inhibitors, we also accept ED males who experienced prior unsuccessful penile venous surgery. Two main causes are identified in unsuccessful conventional penile venous surgery. First, is the incomplete removal of the offending veins in veno-occlusive dysfunction which can be attributed to the antiquated knowledge of penile venous anatomy (Figure 4). Secondly attending surgeon may fail to decline the temptation of applying electrocautery during procedures, causing a catastrophic effect to the delicate corporeal sinusoids. Apart from histology evidence of corporeal fibrosis, cavernosography categorically demonstrated poor filling and uneven distribution of contrast medium due to electrocautery effects from the previous surgery (Figure 5). In this case, penile implantation might be the viable choice because damage to the corporeal sinusoids prevent long term benefits from salvage PVSS.
Figure 4: Cavernosograms of a 29-year-old patient who received prior penile venous surgery elesewhere. (A) The first cavernosogram (anterior− posterior view) was obtained when 10 ml diluted iohexol solution was intracavernously injected into the corpora cavernosa (asterisk) via a no. 19 scalp needle (cross). The preprostatic plexus showed immediate opacification. (B) A 30° oblique-view cavernosogram was obtained after further injection of 10 ml iohexol solution when the deep dorsal vein (arrow) was appropriately visible. Note the venous caliber was smaller distaly owning to a segmental excision in prior surgery. These complex erection-related veins were residual, leftover in prior penile venous surgery? (C) This pharmacocavernosogram revealed veno-occlusive dysfunction via large venous channel (arrow) although prior surgery was undergone elesewhere. (D) Postoperative cavernosogram was obtained after salvaging penile venous stripping. Note the residual veins are no longer present for comparison with panel A with same condition of imaging process. (E) This oblique cavernosogram was obtained for comparison with panel B. Note that the previous residual veins (arrow) were null. (F) Later stage cavernosogram was obtained while an intracorporeal fluid retension was considerably more reacheable. Again the residual veins (arrow) are no longer seen, indicating that an appropriate surgery was performed.
▪ Outcomes of penile venous stripping
Table 2 detail the operative outcome of the PVSS procedure since 1986. Table 3 shows a preliminary analysis of general ED males, and the young ED males under the age of 30 who received PVSS between 2009 and 2015. The ability of intracorporeal fluid retention is dramatically improved regardless of whether it was the first PVSS or a salvaging PVSS (Figure 5). We even acknowledged that the psychological outcome for young ED males was better than the older counterpart. Our PVSS procedure was granted with a USPTO, United States Patent and Trade Office, patent in 2012 [73]. A more favorable outcome can be expected in the majority of venogenic ED patients. This procedure warrants further scientific study through a randomized trial to provide additional robust proof.
| Methods | Patients | Presentation | Follow-up period (years) |
|||||
|---|---|---|---|---|---|---|---|---|
| No. | Age (Year) |
Time period | Op. time (hours) |
IR* (%) |
SR* (%) |
Anatomy blueprint [Reference] | ||
| Ligation | 8 | 22-58 | Jun. 1986 Aug. 1987 |
0.5-2.0 | <50.0 | 0.0 | 5.0-17.0 | Multiple ligation of single DDV*[14,15] |
| Stripping | 23 | 19-68 | Sep. 1986 May 1987 |
2.0-5.0 | 80.0 | 52.5 | 5.0-17.0 | Venous stripping as much as possible [14,15] |
| Stripping | 245 | 19-83 | Jun. 1987 April 1991 |
2.2-3.1 | 67.8 | NA | Venous stripping under local anesthesia since 1988 [62] | |
| Stripping | 1207 | 22-82 | May 1992 Aug. 1997 |
2-3 | 69.7 | 57.6 | Single DDV* with its branches | |
| Stripping | 615 | 23-83 | Sep. 1997 July 2000 |
2-5 | 85.0 | 64.6 | IIEF* available since 1998 Suspected penile venous anatomy |
|
| Stripping | 378 | 19-81 | Aug. 2000 Nov. 2003 |
2.1-5.0 | 90.4 | 76.6 | 5.1-8.2 | Sure penile venous anatomy [17,59,61] |
| Stripping | 235 | 20-91 | Jan. 2004 Jan. 2009 |
2.1-6.2 | 90.8 | 77.8 | DDV*, CV* & PAV* | |
| Stripping | 103 | Feb. 2009 Jan.2011 |
4.2-8.0 | 88.7 | 68.7 | Without well-trained assistant | ||
| Ultimate | 255 | 20-75 | Feb. 2011 Oct. 2015 |
2.1-7.5 | 95.7 | 85.3 | Unpublished data, ultimate method of USPTO patent [73] | |
| Total | 3069 | 19-91 | 0.5-8.0 | <50-95.7 | 0-85.3 | 5-17 | ||
* The DDV, CV, PAV, IIEF, IR & SR are an abbreviation for the deep dorsal vein, cavernosal veins, para-arterial veins,
international index of erectile function, improvement rate and satisfaction rate respectively.
Table 2. Chronological refinement in penile venous stripping surgery methods since 1986.
| Grouping | Patient | IIEF-5# scores | PDE-5# inhibitors | Implant | ICI† | ||||
|---|---|---|---|---|---|---|---|---|---|
| No. | Age | Pre-op | Post-op (1) | Post-op (2) | |||||
| Young group | 46 | 20-30 | 10.2±3.6 | 19.1±3.2 | 21.3±1.7 | 5 | 1 | 2 | |
| Older group | 237 | 31-81 | 9.7±3.8 | 16.4±3.0 | 18.2±3.2 | 47 | 11 | 9 | |
| Total | 283 | 15 | 11 | 11 | |||||
| P-Value* | NA | NS | <0.03 | <0.03 | <0.001 | <0.001 | < 0.001 | ||
*Univariate comparisons were performed using the Student’s t test or Mann-Whitney U test for continuous
Variables wherever appropriate. Chi square test was used for categorical variables.
# IIEF: International Index of erectile function; PDE-5: phosphodiesterase-5;
post-op (1): follow-up at 6 months; post-op (2): follow-up at least one year.
†ICI: intracavernosal injection of the prostaglandin-E1 etc.
Table 3: Summary of 283 patients who underwent penile venous stripping surgery from 2009 to 2015.
Figure 5: Dual pharmaco-cavernosography of a 26-year-old patient who received prior penile venous surgery internationally. (A) The first cavernosogram (anterior−posterior view) was obtained when 10 ml diluted iohexol solution was injected into the corpora cavernosa (asterisk) via a no. 19 scalp needle (cross). Note that the radio-density of the distal corpora cavernosa (asterisk) was lesser than that of the penile crura although the preprostatic plexus showed a few residual veins only. (B) A 30° oblique-view cavernosogram was obtained after further injection of 10 ml iohexol solution while residual veins remain less. Again the radio-density of the distal corpora cavernosa was lesser than that of the proximal portion (asterisk) including the penile crura where electrocautery effect was not susceptible. (C) This pharmaco-cavernosogram revealed uneven radio-density and dentations along the dorsal aspect of the corpora cavernosa (distal to the asterisk mark). (D) Postoperative cavernosogram was obtained after salvaging penile venous stripping. Note the residual veins are no longer present for comparison with panel A with the same condition of imaging processing. (E) This oblique cavernosogram was obtained for comparison with panel B. Note that the intracorporeal fluid retention is dramatically improved, markedly in penile crura. (F) Later stage cavernosogram was obtained while an intracorporeal fluid retention was considerably more reachable.
Discussion
Penile morphology and erectile rigidity are vital for performing genital coitus. Males with psychological stress caused by congenital penile deviation and ED who have benefitted from penile curvature correction (debuted in 1965) and penile implantation (modern type, introduced in the 1950s) are commonly encountered [74,75]. The outer longitudinal layer of the tunica albugenia is the surgery target for both procedures; however, the architecture of the tunical anatomy was discovered as late as 1991[76]. For many years, physicians have endeavored to develop methods to meet patient requirements [77,78]. Intricate tunical surgery should not be regarded as a simple urological task because unfavorable postoperative outcomes may result from this surgery [79]. Furthermore, despite the current trend in ED medical treatment, the number of penile implants performed in the USA continues to increase [80].
A thorough understanding of the rudimentary anatomical knowledge is a prerequisite for the surgeons to successfully perform a surgery that aims to prevent the expenditure of both prosthesis extrusion and revision of unsuccessful corporoplasty [81,82].
In the chronological experience of PVSS, we use the term young ED to refer to males with ED younger than 30 years of age, whereas the borderline age is 40 in medical literature. This arbitrary definition may lead the ED in young males to be attributed to psychogenic causes. An analysis of our patients undergoing PVSS between 2009 and 2015 revealed that gratifying outcomes were as high as 80.5 % (42/52) in young men with ED under the age of 30, the remaining 19.5% continued to have ED, although an improvement was observed. Postoperatively, a 28-year-old man with ED tenaciously tried to present ED complaints; in failing to screen his psychological factor preoperatively it implies that a psychological origin plays a certain role in this group.
Given that the penile veins play a pivotal role in a rigid erection, is it justified to exclude venogenic origin from the list of ED contributors only because conventional penile venous surgery had been ineffective for so long [66]? The importance of the venous contribution to erection is fundamental since it accounts for more than 90% of the ED cases in previous research [6,7]. With this in mind shouldn’t it be the first one on the ED contributor list? The psychological origin has been over-exaggerated in ED because it inadequately explains 42% of ED cases but is still regarded as the main contributor despite known venogenic factors. Penile venous surgery has likely been innocently condemned; the abandonment would be more appropriate if its justification shifted from the surgery itself to the method of surgical manipulation. We heretofore suggest its ban should be lifted to help males that suffer from ED. Surely its efficacy and safety warrant well-structured, randomized, and controlled research by surgeons who know the anatomy well and are well-equipped with microvascular surgery skill without the necessity of electrocautery.
The ED contributor list includes psychogenic, neurogenic, endocrinologic, and arteriogenic, as well as abnormal function of the sinusoidal and cavernosal tissue, structural alterations, degenerative changes, traumatic injury to the tunica albuginea and pharmacological influences. It is difficult to agree that a venogenic contributor is equivalent to a cavernosal factor. It may be beyond the scope of our hemodynamic study since cadaveric intracorporeal tissue cannot meet the viability criteria. Intracorporeal smooth muscle fibrosis has been reported as a major mechanism of venous leakage which may also be a concern that demands a solution [83].
Given that an organic origin plays a central role in young patients afflicted with ED, it is critical that physicians and ED researchers alike recognize and understand newfound knowledge of penile anatomy and erection physiology, including the vascular physiology and pathophysiology for impotence, as well as the notion that the penile erection is, at its core, a mechanical event [84,85]. Such anatomical insights are inspired by—and in turn enhance—clinical applications routinely encountered by researchers and physicians. Viz., this knowledge is highly valuable to surgeons who perform penile morphological reconstruction via autologous venous patched surgery [86], penile implantation with glans sinusoidal enhancement, penile vascular surgery [87], and even penile enhancement surgery (in particular on the glans penis and for penile girth) [88]. These operations are mostly done with an acupuncture assisted local anesthesia and on an ambulatory basis.
Conclusions
ED in males under 30 can be caused by organic and psychogenic factors. Over the last few decades, with advances in our understanding of penile tunical, venous anatomy, erectile physiology and ED pathophysiology, ED therapy can be improved. Despite our belief that penile veins are the principal component in erectile rigidity through our cadaveric hemodynamic studies, we should not ignore the possible existence of a psychological cause of this problem in clinical settings.
Acknowledgement
We would like to thank Nicholas Bagnall for English editing, and Director Chih-Chung Lu, Ms Hsiu-Chen Lu, Ying-Hui Chen for preparing the illustration and photos in this manuscript.
References
- Andersson KE, Wagner G. Physiology of penile erection. Physiol. Rev 75(1), 191–218 (1995).
- Kaminetsky J. Epidemiology and pathophysiology of male sexual dysfunction. Int. J. Impot. Res 20(1), 3–10, (2008).
- Melman A, Gingell JC. The epidemiology and pathophysiology of erectile dysfunction. J. Urol 161(1), 5–11 (1999).
- Schultheiss D, & Stief CG. Physiology and pathophysiology of erection: consequences for present medical therapy of erectile dysfunction. Andrologia31(1), 59-64 (1999).
- Dean RC, Lue TF. Physiology of penile erection and pathophysiology of erectile dysfunction. Urol. Clin. N. Am 32(4), 379–395 (2005).
- Fuchs AM, Mehringer CM, Rajfer J. Anatomy of penile venous drainage in potent and impotent men during cavernosography. J. Urol 141(6), 1353–1356 (1989).
- Elhanbly S, Abdel-Gaber S, Fathy H, et al. Erectile dysfunction in smoker: a penile dynamic and vascular study. J. Androl25(6), 991–995 (2004).
- Rosen RC. Psychogenic erectile dysfunction. Classification and management. Urol. Clin. North. Am 28(2), 269-278 (2001).
- Bodie JA, Beeman WW, Monga M. Psychogenic erectile dysfunction. Int. J. Psychiatry. Med 33(3), 273-293 (2003).
- Capogrosso P, Colicchia M, Ventimiglia E, et al. One patient out of four with newly diagnosed erectile dysfunction is a young man—worrisome picture from the everyday clinical practice. J. Sex. Med 10(7), 1833–1841 (2013).
- Krane RJ, Goldstein I, Saenz de Tejada I. Impotence. N. Engl. J. Med 321(24), 1648-1659 (1989).
- Ludwig W, Phillips M. Organic causes of erectile dysfunction in men under 40. Urol. Int 92(1), 1-6 (2014).
- Papagiannopoulos D, Khare N, Nehra A. Evaluation of young men with organic erectile dysfunction. Asian. J. Androl 17(1), 11–16 (2015).
- Tsai TC, Hsu GL, Chen SC, et al. Analysis of the results of reconstructive surgery for vasculogenic impotence. Taiwan Yi. Xue .Hui. Za. Zhi 87(2), 182-187 (1988).
- Chen SC, Hsieh CH, Hsu GL, et al. The progression of the penile vein: could it be recurrent? J. Androl 26(1), 53-60 (2005).
- Wen HS, Hsieh CH, Hsu GL, et al. The synergism of penile venous surgery and oral sildenafil in treating patients with erectile dysfunction. Int. J .Androl 28(5), 297-303 (2005).
- Hsu GL, Chen HS, Hsieh CH, Lee WY, Chen KL et al. Clinical experience of a refined penile venous stripping surgery procedure for patients with erectile dysfunction: is it a viable option? J .Androl 31(3), 271-280 (2010).
- Hsieh CH, Wang CJ, Hsu GL, et al. Penile veins play a pivotal role in erection: the hemodynamic evidence. Int. J .Androl 28(2), 88–92 (2005).
- Hsu GL, Hung YP, Tsai MH, et al. Penile veins are the principal component in erectile rigidity: a study of penile venous stripping on defrosted human cadavers. J. Androl 33(6), 1176-1185 (2012).
- Holstege G, Georgiadis JR, Paans AM, et al. Brain activation during human male ejaculation. J. Neurosci 23(27), 9185-9193 (2003).
- Georgiadis JR, Holstege G. Human brain activation during sexual stimulation of the penis. J. Comp. Neurol 493(1), 33-38 (2005).
- Miyagawa Y, Tsujimura A, Fujita K, et al. Differential brain processing of audiovisual sexual stimuli in men: comparative positron emission tomography study of the initiation and maintenance of penile erection during sexual arousal. Neuroimage 36(3), 830-842 (2007).
- Georgiadis JR, Kortekaas R, Kuipers R, et al.Regional cerebral blood flow changes associated with clitorally induced orgasm in healthy women. Eur. J. Neurosci 24(11), 3305-3316 (2006).
- Kriegeskorte N, Goebel R, Bandettini P. Information-based functional brain mapping. PNAS 103(10), 3863-3868 (2006).
- Lazar SW, Bush CG, Gollub RL, et al. Functional brain mapping of the relaxation response and meditation. NeuroReport 11(7), 1581-1585 (2000).
- Redoute J, Stoleru S, Gregoire MC, et al. Brain processing of visual sexual stimuli in human males. Human. Brain. Mapping 11(3), 162-177 (2000).
- Arnow BA, Desmond JE, Banner LL, et al. Brain activation and sexual arousal in healthy, heterosexual males. Brain 125(Pt 5), 1014-23 (2002).
- Shamdasani S. Psychotherapy: the invention of a word. History. Of. the. Human. Sciences 18(1), 1–22 (2005).
- Carlson E, Dain N. The Psychotherapy that was Moral Treatment. Am. J. Psychiatry 117(6), 519-524 (1960).
- Specter M. The power of nothing: could studying the placebo effect change the way we think about medicine? New. Yorker 87(40), 1-8 (2011).
- Althof SE, Wieder M. Psychotherapy for erectile dysfunction: now more relevant than ever. Endocrine 23 (2-3), 131-134 (2004).
- Lewis DW, Winner P, Wasiewski W. The placebo responder rate in children and adolescents. Headache 45(3), 232-239 (2005).
- Fernandes R, Ferreira JJ, Sampaio C. The placebo response in studies of acute migraine. J. Pediatr 152(4), 527-533 (2008).
- Cohen D, Consoli A, Bodeau N, et al. Predictors of placebo response in randomized controlled trials of psychotropic drugs for children and adolescents with internalizing disorders. J. Child. Adolesc. Psychopharmacol 20(1), 39-47 (2010).
- Giuliano F, Jackson G, Montorsi F, et al. Safety of sildenafil citrate: review of 67 double-blind placebo-controlled trials and the postmarketing safety database. Int. J. Clin. Pract 64(2), 240-255 (2010).
- Chen KK, Jiann BP, Lin JSN, et al. Efficacy and safety of on‐demand oral tadalafil in the treatment of men with erectile dysfunction in Taiwan: A randomized, double‐blind, parallel, placebo‐controlled clinical study. J. Sex .Med 1(2), 201-208 (2004)
- McCullough AR, Barada JH, Fawzy A, et al. Achieving treatment optimization with sildenafil citrate (Viagra) in patients with erectile dysfunction. Urology 60(2), 28-38 (2002).
- Sivalingam S, Hashim H, Schwaibold H. An overview of the diagnosis and treatment of erectile dysfunction. Drugs 66(18), 2339-2355 (2006).
- Althof SE, Leiblum SR, Chevret-Measson M, et al. Psychological and interpersonal dimensions of sexual function and dysfunction. J. Sex. Med 2(6), 793-800 (2005).
- Berry MD. The History and Evolution of Sex Therapy and its Relationship to Psychoanalysis. Int. J. Applied. Psychoanalytic. Studies 10(1), 53-74 (2013).
- Shah J. Erectile dysfunction through the ages. BJU Int 90(4), 433-441 (2002).
- Li CL. A brief outline of Chinese medical history with particular reference to acupuncture. Perspect. Biol. Med 18(1), 132–143 (1974).
- Bella AJ, Shamloul R. Traditional plant aphrodisiacs and male sexual dysfunction. Phytother. Res 28(6), 831-835 (2014).
- Hsieh CH, Tai HC, Hsu GL, et al. Herb formula enhances treatment of impotent patients after penile venous stripping, a randomized clinical trial. Andrologia 48(7), 754-760 (2016).
- Shamloul R. Natural Aphrodisiacs. J. Sex. Med 7(1 pt 1), 39-49 (2010).
- Silverman DK. What Works in Psychotherapy and How Do We Know? What Evidence-Based Practice Has to Offer? Psychoanalytic. Psychology 22(2), 306–312 (2005).
- Simopoulos EF, Trinidad AC. Male erectile dysfunction: integrating psychopharmacology and psychotherapy. Gen. Hosp. Psychiatry 35(1), 33-38 (2013).
- Eysenck H. The effects of psychotherapy: An evaluation. J .Consult .Psychol 16(5), 319–324 (1952).
- Brotto L, Atallah S, Johnson-Agbakwu C, et al. Psychological and Interpersonal Dimensions of Sexual Function and Dysfunction. J .Sex. Med 13(4), 538-571 (2016).
- Hublin JJ, Ben-Ncer A, Bailey SE, et al. New fossils from Jebel Irhoud, Morocco and the pan-African origin of Homo sapiens. Nature 546 (7657), 289–292 (2017).
- Eardley I, Sethia K. In Anatomy and physiology of erection. Erectile dysfunction, current investigation and management. 7-23 Mosby, London, 2003.
- Hsu GL, Brock G, von Heyden B, et al. The three-dimensional structure of the human tunica albuginea: anatomical and ultrastructural level. Int. J. Impot. Res 4, 117-129 (1992).
- Hsu GL, Hsieh CH, Wen HS, et al. Penile venous anatomy: an additional description and its clinical implication. J. Androl 24(6), 921-927 (2003).
- Hsu GL, Lin CW, Hsieh CH, et al. Distal ligament in human glans: a comparative study of penile architecture. J. Androl 26(5), 624-628 (2005).
- Hsu GL, Hsieh CH, Wen HS, et al. Anatomy of the human penis: The relationship of the architecture between skeletal and smooth muscles. J. Androl 25(3), 426-431 (2004).
- Hsieh CH, Liu SP, Hsu GL Chen HS, et al. Advances in our understanding of mammalian penile evolution, human penile anatomy and human erection physiology: Clinical implications for physicians and surgeons. Med. Sci. Monit 18(7), RA118-125 (2012).
- Hsu GL, Hsieh CH, Wen HS, et al. Formulas for determining the dimensions of venous graft required for penile curvature correction. Int. J. Androl 29(5), 515-520, (2006).
- Hsu GL, Chen HS, Huang SJ. Does tunica anatomy matter in penile implant? Transl. Androl. Urol4(4), 406-412 (2014).
- Hsu GL, Hsieh CH, Wen HS, et al. Outpatient penile implantation with the patient under a novel method of crural block. Int. J. Androl 27(3), 147-151 (2004).
- Hsu GL, Chen HS, Hsieh CH, et al. Long-term result of an autologous venous grafting for penile morphological reconstruction. J. Androl 28(1), 186-193 (2007).
- Hsu GL, Hsieh CH, Wen HS, et al. Outpatient surgery for penile venous patch with the patient under local anesthesia. J. Androl 24(1), 35-39, (2003).
- Hsu GL, Molodysky E, Liu SP, et al. Reconstructive surgery for idealizing penile shape and erectile functional restoration on patients with penile dysmorphology and erectile dysfunction. Arab. J. Urol 11(4), 375–383 (2013).
- Hsu GL, Huang YP, Tsai MH, et al. The venous drainage of the corpora cavernosa in the human penis. Arab. J. Urol11(4), 384-391 (2013).
- Hsieh CH, Huang YP, Tsai MH, et al. Tunical Outer Layer Plays an Essential Role in Penile veno-occlusive Mechanism Evidenced from Electrocautery Effects to the Corpora Cavernosa in Defrosted Human Cadavers. Urology 86(6), 1129-1136 (2015).
- Parona F. Imperfect penile erection due to varicosity of the dorsal vein: observation. Giornale. Italiano. Delle. Malattie. Veneree. E. Della. Pelle 14, 71-76 (1873).
- Wooten JS. Ligation of the dorsal vein of the penis as a cure for atonic impotence. Tex. State. Med. J18, 325-328 (1902).
- Lowsley OS, Rueda A. Further experience with anoperation for the cure of certain types of impotence. J. Int. Coll. Surg 19(1), 69-77 (1953).
- Wespes E, Schulma CC. Venous leakage: surgical treatment of a curable cause of impotence. J. Urol 133(5), 796-8 (1985).
- Montague DK, Barada JH, Belker AM, et al.Clinical guidelines panel on erectile dysfunction: summary report on the treatment of organic erectile dysfunction. J. Urol156(6), 2007-2011 (1996).
- Hwang TI, Yang CR. Penile vein ligation for venogenic impotence. Eur. Urol 26 (1), 46-51 (1994).
- Hsu GL, Chen HS, Hsieh CH, et al. Salvaging Penile Venous Stripping Surgery. J. Androl 31(3), 250-260 (2010).
- Hatzimouratidis K, Eardley I, Giuliano F, et al. Guidelines on male sexual dysfunction: erectile dysfunction and premature ejaculation. 2014, European Association of Urology,.
- Hsu GL. Physiological approach to penile venous stripping surgical procedure for patients with erectile dysfunction. Google Patents; Patent No: US 8,240,313 B2,.
- Nesbit RM. Congenital curvature of the phallus: report of three cases with description of corrective operation. J. Urol 93(2), 230-232 (1965).
- Goodman WE. & Scott WW. Phalloplasty. J. Urol 68(6), 903-908 (1952).
- Hinman Jr F. Penis and male urethra. In Atalas. Of. UroSurgical. Anatomy. 432-433 (WB Saunders, 1993).
- Ebbehøj J, Metz P. Congenital penile angulation. Br. J. Urol 60(3), 165-166 (1987).
- Yachia D. Modifiedcorporoplasty for treatment of penile curvature. J. Urol 143(1), 80-82 (1990).
- Alvaro Paez, Juan Mejias, Jorge Vallejo, et al. Long-Term Patient Satisfaction after Surgical Correction of Penile Curvature via Tunical Plication. Int. Braz. J .Urol 33(4), 502-509 (2007).
- Montague DK. Penile prosthesis implantation in the era of medical treatmentfor erectile dysfunction. Urol. Clin. North. Am 38(2), 217–225 (2011).
- Hsu GL, Brock G, Martinez-Pineiro L, et al. Anatomy and strength of the tunica albuginea: its relevance to penile prosthesis extrusion. J. Urol 151(5), 1205-8 (1994).
- Hsieh CH, Chen HS, Lee WY, et al. Salvage Penile tunical surgery. J. Androl 31(5), 450-456 (2010).
- Nehra A, Goldstein I, Pabby A, et al. Mechanisms of venous leakage: a prospective clinicopathological correlation of corporeal function and structure. J. Urol 156(4), 1320–1329 (1996).
- Hsu GL, Liu SP. Male Reproduction tract: penis structure. Chapter 59, Volume 1. In: Skinner AM, Niederberger C, Valles CS, Jégou B, Flaws J, McCarry J, Spencer T, Swanson P, Wen Y, editors. Reproduction. Encyclopedia. Second. edition, Amsterdam, Elsevier 2018. (Accepted)
- Hsu GL, Lu HC. Male Reproduction tract: penis structure-Erection, Chapter 60, Volume 1. In: Skinner AM, Niederberger C, Valles CS, Jégou B, Flaws J, McCarry J, Spencer T, Swanson P, Wen Y, editors. Reproduction. Encyclopedia. Second. Edition Amsterdam, Elsevier 2018. (Accepted)
- Hsu GL, Lu HC. Male Reproduction tract: Erection abnormality, Chapter 62, Volume 1. In: Skinner AM, Niederberger C, Valles CS, Jégou B, Flaws J, McCarry J, Spencer T, Swanson P, Wen Y, editors. Reproduction. Encyclopedia. Second. edition Amsterdam, Elsevier 2018. (Accepted)
- Huang PC, Hsu GL. Vascular surgery for erectile dysfunction, Chapter 79, Volume 4. In: Skinner AM, Niederberger C, Valles CS, Jégou B, Flaws J, McCarry J, Spencer T, Swanson P, Wen Y, editors. Reproduction. Encyclopedia. Second. editio, Amsterdam, Elsevier 2018. (Accepted).
- Hsu GL, Hill JW, Hsieh CH, et al. Venous ligation: A novel strategy for glans enhancement in penile prosthesis implantation. Biomed. Res. Int Volume 2014 (2014).