Research Article - (2023) Volume 13, Issue 6
Insomnia Insights: A Retrospective Study of Sleep Patterns at Kuwait Centre for Mental Health over 16 years.
- Corresponding Author:
- Mohamed Binali,
Department of psychiatry, Kuwait Centre for mental health, Kuwait
E-mail: [email protected]
Received date: 25-Dec-2023, Manuscript No.NPY-23-123429; Editor assigned: 27-Dec-2023, PreQC No.NPY-23-123429 (PQ); Reviewed date: 10-Jan-2024, QC No.NPY-23-123429; Revised date: 17-Jan-2024, Manuscript No.NPY-23-123429 (R); Published date: 24-Jan-2024, DOI: 10.37532/1758-2008.2023.13(2).685
Abstract
Chronic insomnia is often presented with many medical and psychiatric disorders, and its underlying aetiology needs to be identified by using Polysomnography (PSG) to achieve safe and effective management. Obstructive Sleep Apnoea (OSA) and Parasomnia such as Limb Movement Disorder (PLMD) are common primary sleep disorders that can lead to chronic insomnia. Patients with chronic insomnia need to be evaluated and managed.
Methods: Across sectional epidemiological study for a total number of 397 patients diagnosed with long history of chronic insomnia with mental disorders using PSG reports as marker, seen at Sleep Disorder Unit in Kuwait Centre for Mental Health (KCMH).
Results: By reviewing PSG montage and reports of 397 individuals, 38.5% of chronic insomnia related to mental illness, 3.5% only related to primary insomnia, 22.1% had Obstructive sleep apnoea, 5.5% had hypersomnia, 5.2% had narcolepsy, 2.77% PLMD, 1.25% had Circadian Rhythm Disorder (CRD) and 5.79% of sample were not done by patients.
Conclusion: Using PSG as a marker for chronic insomnia in individual with mental illness and evaluates the underline cause of chronic insomnia. It is cost effect on the long term and an adequate strategy to treat insomnia among our patients.
Keywords
Insomnia, obstructive sleep apnoea, mental disorders, polysomnography, kuwait centre for mental illness
Introduction
Insomnia as a part of symptomology is seen in the most psychiatric disorders during our practice and is the most reported sleep problem in developing and industrialised countries worldwide. An international survey on sleep problems in the general population showed a high prevalence of insomnia was presented as 23% of Japan populations and insomnia prevalence was presented in 56% of the United States populations and many individuals with insomnia, about 47%-67% did not seek medical attention for their sleep difficulties including individuals with mental illness [1,2].
Unfortunately, the stigma associated with mental illness among patients remain a significant barrier for help‑seeking and treatment adherence and management. As about 40% of all insomnia cases are associated with common psychiatric conditions such as depression or anxiety [3-5]. The International Classification of Sleep Disorders (ICSD‑2) stated there are 55 disorders that include insomnia as one of the complaints and its diagnostic framework identify categories of sleep disorders secondary to medical conditions, substance use and psychiatric disorders [6]. Also, the patient’s underlying medical problems, medications used for treatment and possible substance abuse/dependence are contributing factors to chronic insomnia.
Insomnia is primarily diagnosed by clinical evaluation, through detailed medical, psychiatric and sleep history-taking. But today its remains a largely underdiagnosed and under‑treated problem among patients with daily impairment and difficulties. An Overnight Polysomnography (PSG) is a standard tool and procedure in sleep medicine for evaluating sleep‑related pathophysiology. The American Academy of Sleep Medicine’s (AASM) practice parameters for using PSG recommend using PSG in clinical evaluation of transient insomnia.
There was no previous research done involving psychiatric patients being referred to Sleep Disorder Unit at the Kuwait Centre for Mental Health from the causality, Out Patient Department (OPD) and wards. This is the first retrospective clinical epidemiological study showing the prevalence of the sleep disorders underlining chronic insomnia occurred among patients with mental disorders attending the KCMH (only Psychiatric facility) in the State of Kuwait over the last 16 years. The aims were identifying the underline cause for chronic insomnia by objectively reviewing the Patients PSG reports and identifying the sleep disorders such as Obstructive Sleep Apnoea (OSA), Parodic Limb Movement Disorder (PLMD), Narcolepsy, etc. Also looking at its prevalence among Kuwaiti population and if chronic insomnia were primary or secondary to medical or psychiatric disorders as comorbidities.
Methodology
Study design
This is a retrospective cross sectional clinical epidemiological study that is done for patients who have chronic persistent insomnia referred from different sites and who had done a PSG at Sleep Disorder Unit (SDU) in KCMH in the last 16 years. In this study, the sample selection includes patients diagnosed with long term insomnia which has chronic course, who suffer from mental disorder according to Diagnostic and Statistical Manual of Mental Disorders (DSMV) and has medical comorbidities such as Epilepsy, organic brain syndrome, head trauma, Cerebral Vascular Accident (CVA) and others.
Study setting and location
The study was conducted at Sleep Disorder Unit that is based at 1st floor inside the Kuwait Centre for Mental Health. It is the only Sleep Disorder Unit available in the state of Kuwait that involve in the sleep disorders and its comorbidity with mental disorders. The state of Kuwait located in the Arabian Gulf, part of Gulf Cooperation Council (GCC), in the Middle East. It has a population of 3 million and half according to Government national Data 2021.
Study population
The population samples were drawn from PSG reports, PC sleep montage, the present referral medical letters and patients’ medical files. It has a demographic data such as patient nationality, ethnicity, gender, age, and reason for referral with all aspect of participation. The patient selection was based on having chronic insomnia, mental disorders, being on medical and psychotropic medications and having medical comorbidities. All data was recorded on research Data sheet. The total number was 397 participants, 271 (68.2%) males and 126 (31.7%) females (Males numbers are more than females in the sample that were chosen). There were inclusion criteria: age 16-85 years old, with chronic insomnia (more than 3 months) according to DSMV and ICS-version 3, with or without medical comorbidities on psychotropic medications.
There were exclusion criteria less than 16 years old, ongoing delirium, acute florid psychotic patients such as catatonia, very agitated and violence candidate. This used to set a standard for the patients to involve in the study and ensure their safety when doing PSG. All patients sleep studies were reviewed including sleep study reports and montages. It was done by research team members, who were not involve with patient PSG recording, montaging, and treatment. Some patients did not complete the procedure of PSG and left the sleep lab while recoding procedure. There was no consent taken from the patients and the Informed Consent Statement were not applicable.
Data
It was collected and recorded by team members and nurses on research Data sheet. It was analysed by Statistical Package for the Social Sciences (SPSS) version 25. We used descriptive statistics and analysis method such as tables and bar charts to describe the association between different independent variables such as gender, age, nationality, ethnicity and sleep disorders and mental illness.
Results
The independent variables as shown in Table 1 below are the total number was 397 and there were 4 different age groups. The highest age number was (40.5%) of the sample between 41 years old and 60 years but lowest was among patients aged more than 60 years old (9.1%). Also there were differences in number and percentage among gender; male was 271 (68.3%) and female was 126 (31.7%). Mainly the sample was from Middle East ethnicity (91.6%) and Kuwaiti nationality were 66.5%.
| Variable | No. (%) |
|---|---|
| Age | |
| Less than 20 | 49 (12.3%) |
| 21-40 | 149 (37.5%) |
| 41-60 | 161 (40.5%) |
| More than 60 | 36 (9.1 %) |
| Gender | |
| Male | 271 (68.3%) |
| Female | 126 (31.7%) |
| Ethnicity | |
| Arab | 364 (91.6%) |
| Asian | 34 (8.5%) |
| Nationality | |
| Kuwaiti | 264 (66.5%) |
| Others | 128 (32.2%) |
Table 1: Characteristics of the study population (n=397)
Table 2 below showed the diagnostic outcomes of different sleep disorders after Polysomnography (PSG) in the last 16 years. There were 167 (42%) had chronic insomnia, followed by 88 patients (22.1%) who had Obstructive Sleep apnoea, 23 patients (5.5%) had hypersomnia with narcolepsy disorder was 5.2%.
| PSG Diagnostic Outcome | Number | % |
|---|---|---|
| Obstructive Sleep Apnoea | 88 | 22.10% |
| Insomnia | 167 | 42% |
| Hypersomnia | 23 | 5.5% |
| Narcolepsy | 19 | 5.20% |
| Periodic limb movement disorder | 11 | 2.77% |
| Circadian Rhythm Disorder | 5 | 1.25% |
Table 2: The main sleep disorders among patients diagnosed after PSG study.
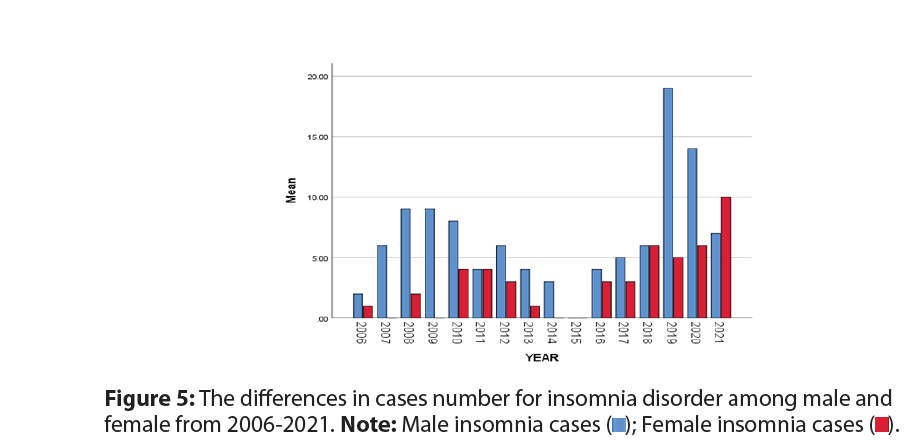
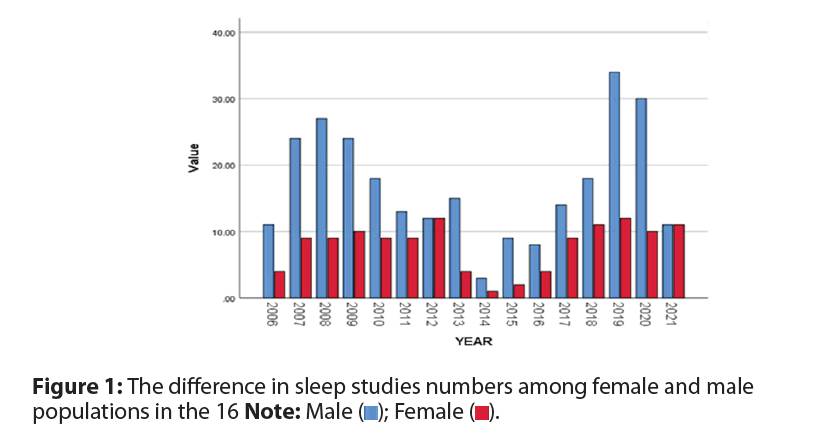
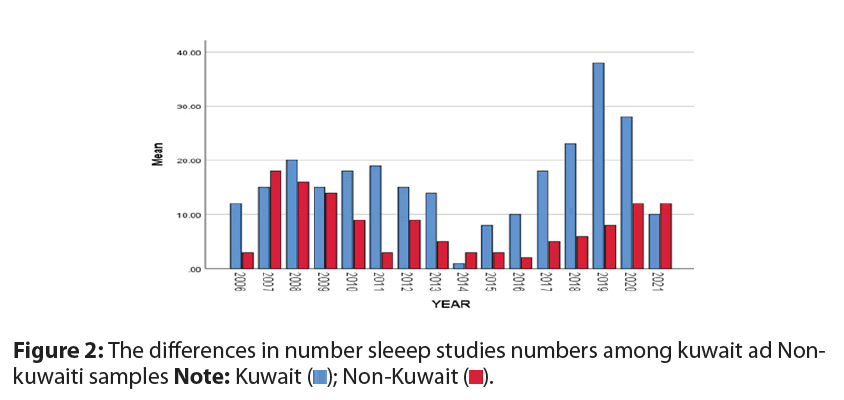
For PLMD, it was 2.77% and for Circadian Rhythm Disorder (CRD) was 1.25%. In the Table 3, it showed the Overview of the diagnostic outcomes after PSG in patients with chronic persistent insomnia underlying psychiatric conditions. All cases were attended by different psychiatrist at Psychiatric OPD and the diagnosis was confirmed and patient were followed up on regular basis. Anxiety (7.5%) and depression (12.6%) were the highest among patients in this study that underline secondary insomnia while the lowest was Adult Attention-Deficit or Hyperactivity Disorder (ADHD) (0.25%). It was 9.8% who had medical conditions comorbid with insomnia. Also, it is suggested that 3.5% of insomnia disorder was primary in this population sample. The Sleep efficacy was less than 85% in all the cases mentioned above, suggesting that 38.5% insomnia was linked to the psychiatric condition such as anxiety, depression, Post-traumatic Stress Disorder (PTSD), psychosis and Substance Use Disorder (SUD), ADHD, Mental retardation, Learning Disability (LD) and medical condition that precipitating mental disorders such as epilepsy, CVA, organic brain syndrome, head trauma and others. Now we will address the results of some of above variables. Figure 1 showed the male sleep studies were higher than female in all years except in 2012 and 2021, female sleep studies were equal to male sleep studies. The highest male sleep studies were in 2019 and lowest were in 2014. Also, the highest female sleep studies were in 2012 and the lowest were in 2014. Figure 2 showed the number of sleep studies that were done for Kuwaiti sample were higher than non-Kuwaiti sample in all years except 2007 and 2014. The highest number was in 2019 for Kuwaiti and in 2007 for non-Kuwaiti population. But the lowest number for Kuwaiti was in 2014 and in 2016 for non-Kuwaiti.
| Attended by psychiatrist | Number (N) | % |
|---|---|---|
| Anxiety disorder | 30 | 7.5% |
| PTSD | 3 | 0.75% |
| Depression | 50 | 12.6% |
| Psychosis | 23 | 5.8% |
| SUD | 4 | 1% |
| Other general medical condition | 39 | 9.8% |
| LD/ Mental retardation | 3 | 0.75% |
| ADHD | 1 | 0.25% |
| Total | 153 | 38.5% as 2nd Insomnia |
| Insomnia in general | 167 | 42% |
| Primary insomnia | 14 | 3.5% as 1st Insomnia |
Table 3: The diagnostic outcomes after Polysomnography (PSG) in patients with sleep disorder underlying psychiatric conditions over 16 years.
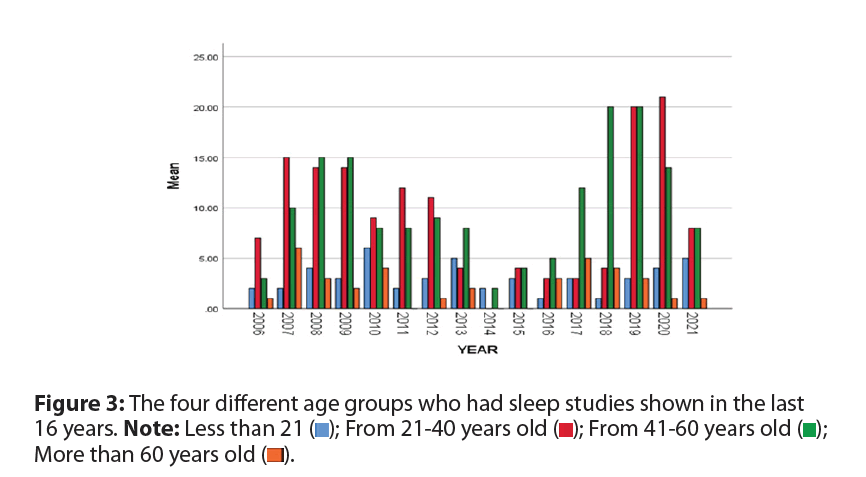
Figure 3 showed the age in years was divided to four groups. The first age group had the highest sleep studies were 3rd group, green colour (from 41 years old to 60 years old) followed by 2nd group, red colour (21 years old to 40 years old), followed by 1st group, blue colour (less than 21 years old), and the last group was 4th group, orange colour (more than 60 years old) who had the lowest number of sleep studies among our population (Circadian rhythm disorder).
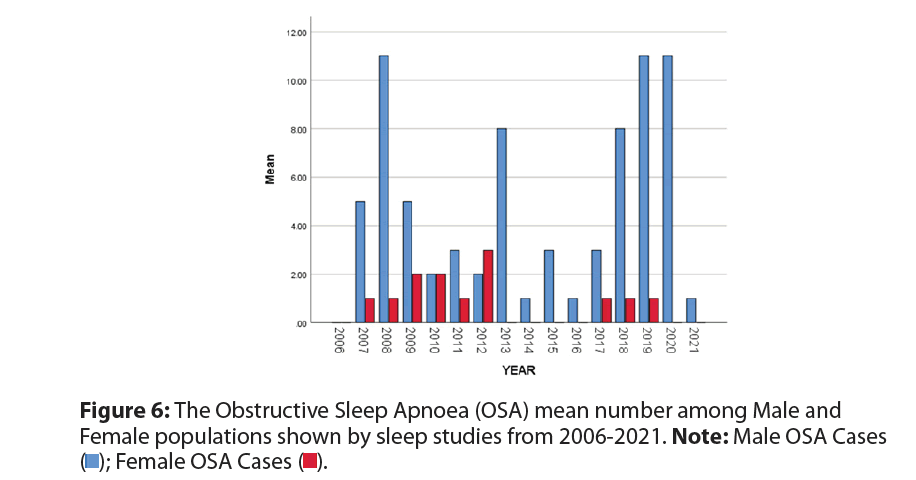
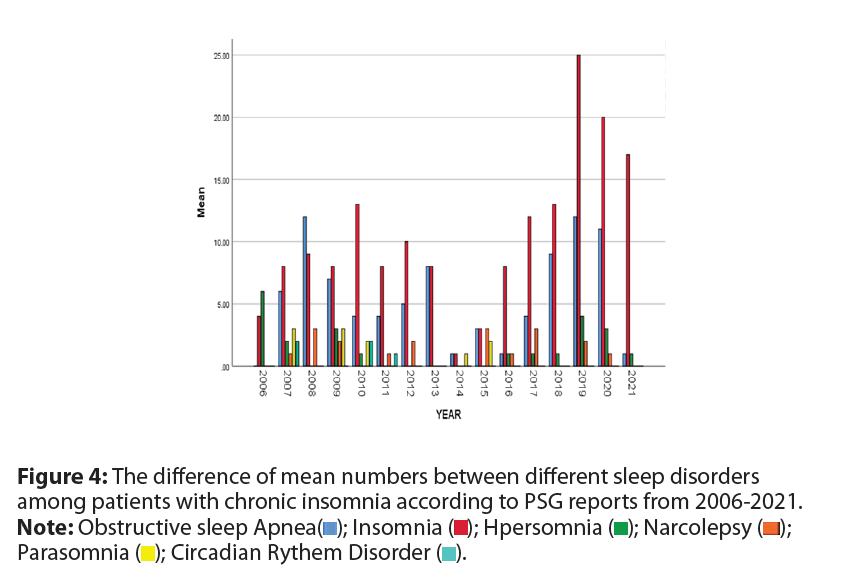
Figure 4 showed sleep studies recorded over 16 years, insomnia disorder was the highest number followed by Obstructive Sleep Disorders (OSA) and the circadian rhythm disorders had the least number. In 2014 and 2015, the number of sleep disorders were the lowest and the highest was in 2019. Figure 5 showed the number of insomnia disorder cases followed sleep studies among male and female populations. The male mean number for insomnia was higher than female mean number all years except in 2021. The mean number of insomnia disorder following sleep studies were equal in 2011 and 2018. Male insomnia disorders were only reported in 2014.
Figure 6 showed the OSA cases number among male and female patients who complained of sleep disturbance and chronic insomnia. The male cases with OSA were higher than female cases with OSA. The highest number for male were in 2008, 2019 and 2020 and the lowest numbers were in 2014, 2016 and 2021. Also, the highest number of cases for female were in 2012 and the lowest were in 2007, 2008, 2011, 2017, 2018 and 2019. There were no Female OSA cases founded in 2014, 2015, 2016, 2020 and 2021.
Discussion
This is the first study done according to our researches data in state of Kuwait involving mental ill patients who had been referred for PSG study for chronic insomnia at Sleep Disorder Unit (SDU) based at Kuwait Centre for Mental Health. The number of patients were referred has been increasing steadily and was due to the introduction of our local Clinical Practice Guidelines (CPGs) for the prescription of benzodiazepines by the Ministry of Health in Kuwait in 2006 and which resulted in our psychiatrist making more patient referrals rather than prescribing potentially addictive hypnotics.
With the increase in the number of psychiatrists supporting the SDU in the past years, patients referred for insomnia have been preferentially channelled to their OPD clinics; since 2006. Almost all patients referred to the SDU for only the stated complaint of on going chronic insomnia were sent to psychiatrists. Psychiatrists have advantage over other specialists in assessing patients with insomnia, as they have an additional repertoire of clinical skills to assess psychological issues that may have contributed to the condition of these patients [7].
There were also patients who had no clear psychological reasons for their sleep complaints and were not responding to sleep medications. In such cases, a recommendation for a sleep study is warranted.
The referring primary care physician may not have identified these symptoms or did not indicate them in the referrals. Most patients were referred from KCMH causality and OPD at KCMH and some patients would have benefitted from PSG evaluation but declined it, due to site based at KCMH as reason. Symptoms and features suspicious of primary sleep disorders can often be elicited in these patients. In the present study, almost 397 patients were (age range 16 to 85 years old). Bar in mind, the Patients who are age from 30 to 69 are more likely to be economically active and stable, as compared to those in their twenties (who are likely at the start of their careers).
They may be more concerned about the impact of insomnia on their health and less tolerant to the physical effects of chronic insomnia on daytime function (e.g. reduced job performance). This explanation could only be based on reasonable assumptions, as the present study is a retrospective one and information about the patients’ employment and socioeconomic status (obtained from their case records) was insufficient. Similarly, the observation showed more male patients underwent the sleep study as compared to female patients could be related to employment and cultural status.
It is possible that some women homemakers did not view daytime impairment from insomnia to be as critical as those who would be appraised negatively for poor work performance [1]. As such, these women might not have seen the need for a sleep study, but instead made behavioural changes (e.g. taking more naps in the day) to adapt. While current evidence shows that chronic insomnia is more common in elderly and female populations this is in reference to the general population and not a clinical population, as in the present study [8,9].
An overview of the PSG sleep indices revealed that our study population had poor sleep characteristics in general. In the present study, only 42% patients were suspected of having primary insomnia based on clinical consultation. In contrast, this number was 47.5% in the study conducted by Mahendran et al., [9]. But instead, only 3.5% had primary insomnia and 38.5% has insomnia secondary to mental illness in this study. Meanwhile, in another study showed 40% of those with insomnia and 46.5% of those with hypersomnia had a psychiatric disorder compared with 16.4% of those with no sleep complaints.
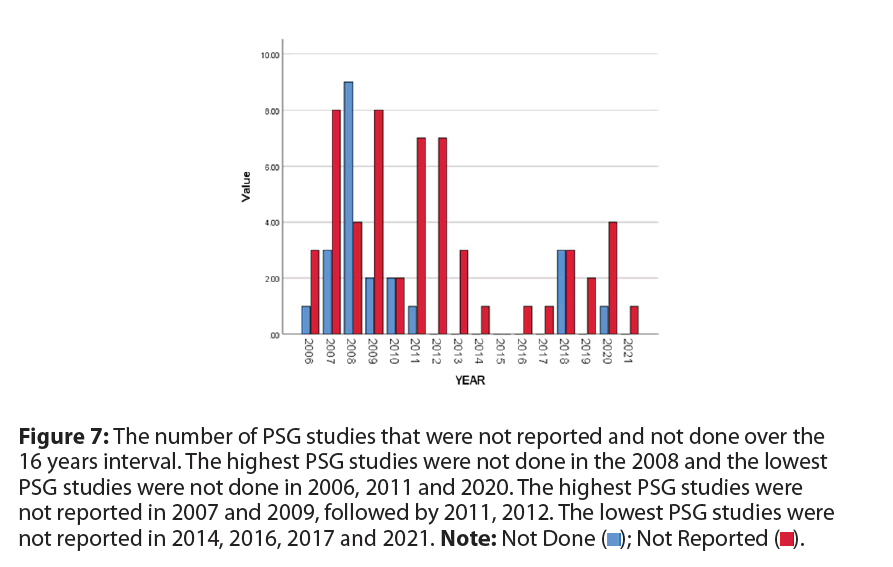
The proportion of patients in SDU who have primary insomnia is likely to be even higher, as 5.79% were clinically diagnosed with chronic insomnia may have declined PSG studies because they did not complete the procedure and 13.85% of the PSG reports were not done due to IT malfuncation and PSG breakdown (Figure 7).
Figure 7: The number of PSG studies that were not reported and not done over the
16 years interval. The highest PSG studies were not done in the 2008 and the lowest
PSG studies were not done in 2006, 2011 and 2020. The highest PSG studies were
not reported in 2007 and 2009, followed by 2011, 2012. The lowest PSG studies were
not reported in 2014, 2016, 2017 and 2021. Note: Not Done ( ); Not Reported (
); Not Reported ( ).
).
The present study was not without limitations.
The population in this retrospective study was highly selective and may represent patients who have severe psychological distress and or dysfunction from their sleep disturbances, or have poor tolerance to such distress. Referral bias is significant in the present study, as the patients identified were highly self-selected and agreed to PSG evaluation. Some patients declined further evaluation with PSG due to social reasons or contentment with ‘quick-fix’ medications, even though their clinical histories were suspicious for the presence of sleep disorders.
Furthermore, about 40% of the 82% of patients who were suspected to have insomnia by PSG that showed insomnia due to the presence of different sleep disorders.
The total number of the sample was 397 and there were 4 different age groups. The highest age number was between 41 years old and 60 years Baring in mind that Patients aged 30 to 69, are more likely to be economically active more dependent upon and more stable, as compared to those in their twenties (who are likely at the start of their careers). They may be more concerned about the impact of insomnia on their health and less tolerant to the physical effects of chronic insomnia on daytime function (e.g. reduced energy as a whole and job performance) but the lowest was among patients aged more than 60 years old. Also there were differences in number and percentage among gender male was 271 and female was 126.
This explanation could only be based on reasonable assumptions, as the present study is a retrospective one and information about the patients’ employment and socioeconomic status (obtained from their case records) was insufficient. In other studies showed Gender diferences and couples sleep were affected by intersecting social and societal infuences, which supports a socio-ecological approach to sleep [10,11]. Similarly, the observation: more male patients underwent the sleep study as compared to female patients could be related to socio-economic status [11].
It is possible that some women homemakers did not view daytime impairment from insomnia to be as critical as those who would be appraised negatively for poor work performance. Studies of insomnia support a female predominance, with increased divergence of prevalence between men and women with older age [10]. In one study by Tang et al., showed that female gender, older age, higher level of education, being unmarried, living in the rural area, cigarette smoking and alcohol drinking were associated with insomnia [12]. It provide important information for general and mental health research.
As such, these women might not have seen the need for a sleep study, but instead made behavioural changes (e.g. taking more naps in the day) to adapt and it developed during pregnancy and child birth [13]. Mainly the study sample was from Middle East ethnicity (91.6%) and Kuwaiti nationality were 66.5%.In the present study, the diagnostic outcomes of different sleep disorders after Polysomnography (PSG) in the last 16 years, were 167 (42%) patient diagnosed with only chronic insomnia, followed by 88 patients (22.1%) diagnosed with Obstructive Sleep apnoea, while 23 patients (5.5%) had hypersomnia with narcolepsy disorder scoring 5.2% of the whole sample.
Most patients attending sleep clinic were referred from KCMH causality and OPD at KCMH. Also many patients would have benefitted from PSG evaluation but declined it, due to site based at KCMH and inconvenience as reasons. Symptoms and features suspicious of primary sleep disorders can often be elicited in these patients. Our results in the current study in hand was very near to one done in Singapore where they studied PSG records of 106 patients with chronic insomnia who presented to a multidisciplinary sleep clinic in Singapore 2015 by Sheau-Hwa Wong, over a five-year period. Which found among a 106 patients they studied, a 69 (65.4%) to have primary sleep disorders (insomnia) based on clinical history and examination alone, and 45 (42.5%) patients showing evidence of OSA upon PSG, and 5 (4.7%) were found to have positive PSG findings for PLMD. And the other 19 (17.9%) were found to have possible sleep state misperception, conditioned insomnia, or poor sleep efficiency.
In addition we found one local study conducted by Mahendran et al., who reviewed all patients referred to their insomnia clinic of psychiatric service over a period of three years and found that 52.9% of those patients were referred due to the insistence of the referring physician and that 54.2% of them had had sleep problems mainly insomnia for more than a year and obstructive sleep apnea. Also while reviewing epidemiological insomnia studies we came through one study done in 2022 by Kundu et al., who utilized the retrospective laboratory and medical records of two groups of patients; chronic insomnia and OSA [14]. Sleep disorders were diagnosed according to standard criteria. They found that chronic Insomnia and Obstructive Sleep Apnea (OSA) constitute the top two most common sleep-related disorders the thing that matched our work here, but they found that in many cases both conditions to exist comorbidly. In addition, to that they noticed one thing in common to our method and that is Insomnia is primarily diagnosed because of clinical history, while for the diagnosis of OSA, overnight Polysomnography (PSG) is required in addition to clinical features.
While most current evidence shows that chronic insomnia is more common in elderly and female populations, this studies are all in reference to the general population and not to a clinical population, as in our present study [15]. In another study showed a prevalence of chronic insomnia in 33% in the sample population surveyed, with females being more affected compared to males but in statistically insignificant values [16]. There was a significant prevalence in patients having diabetes irrespective of the duration of diabetes and drugs taken. Increasing age was also a significant contributor to insomnia in adults. There was no major correlation with education social/economic factors and comorbid conditions such as hypertension, asthma, migraine, heart diseases, and liver or kidney diseases. An overview of the PSG sleep indices revealed that our study population had poor sleep characteristics in general and the mean scores for the different sleep indices (measuring sleep quantity and quality, sleep efficiency, arousals, respiratory abnormalities and motor activities) were in the impaired or abnormal range within psychiatric patients.
In the present study, only 42% patients were suspected of having primary insomnia based on clinical consultation. In contrast, this number was 47.5% in the study conducted by Mahendran et al., [9]. But instead, only 3.5% had primary insomnia and 38.5% has insomnia secondary to mental illness. There is a clear association between insomnia and anxiety and depression mainly among psychiatric populations [17]. The proportion of patients in SDU who have primary insomnia is likely to be even higher, as many patients who were clinically diagnosed with primary insomnia may have declined PSG studies and drop out. One study reported that patients with comorbid OSA and insomnia have significantly higher rates of psychiatric disorders compared with those with only OSA (47.8% vs 28.7% respectively) [18]. Recognizing and managing OSA in patients with psychiatric disorders are crucial to improve response to treatment, quality of life, and overall health. A high proportion of chronic insomnia sufferers in our study have underlying psychiatric illnesses that pose as an alarm and leading to delayed or under diagnosis of primary or secondary sleep disorders, which require different treatments from psychiatric illnesses. In one study showed Insomnia can also be comorbid with other psychiatric disorders, thereby adding to the medical burden and increasing the risk of psychiatric relapse [19].
To sum up, this study showed
• In the present study, targeted use of PSG revealed the presence of common sleep disorders, especially OSA, in a significant proportion (up to 22%) of chronic insomnia sufferers.
• Secondary insomnia was also noted in patients with underlying psychiatric comorbidity nearly 38.5% [17,20].
• Meanwhile the prevalence of insomnia in non-hospitalized psychiatric patients was reported at 43.0% in some studies, which is significantly higher than insomnia in the general population [12].
• We also found that, while at least 80% of the referred patients had sufficient symptoms and features to suggest the presence of sleep disorders other than insomnia disorder, they were not identified by the referring physicians [21].
• This finding is a cause for concern, as it suggests that the referring physicians had inadequate knowledge and training in sleep medicine to effectively manage chronic insomnia.
• This result showed that it is an important and vital process that will allow us to lay down the corner stone for future first sleep centre in the state of Kuwait and provide an establishment way to improve service toward general population.
Conclusion
Identifying the underlying reason for persistent insomnia plays an important role in the treatment and prognosis of the condition. This study showed the importance of PSG in identifying the sleep disorder related to chronic insomnia among mental ill populations in state of Kuwait over 16 years that mainly secondary to mental disorders. It is clear that primary insomnia was the least finding in this research about 3.5% among mental ill patients who were diagnosed with chronic insomnia.
The strategy with which psychiatrists approach patients who present with insomnia may also have differed from that of non‑psychiatrist sleep specialists (due to different emphases and concerns). Physicians should have a comprehensive understanding of the aetiologies of insomnia and be able to make timely referrals for further investigations or goal‑directed specialist interventions. This may have influenced clinical management and stage of illness at which patients entered PSG evaluation. However, in spite of these above limitations, the present study provides important lessons that are applicable in clinical practice because it was based on the observations of a real‑world practice and its efficacy.
The management of insomnia remains an interesting challenge for physicians and psychiatrists. Insomnia is often treated symptomatically at the primary care level even though it is a complex medical condition that may have various underlying aetiologies, resulting in its chronicity. If we consider the above discussion, further research is needed to explore chronic insomnia among psychiatric patients during their illness. This gap in sleep medicine education should be addressed by the medical education system and future sleep centre in the state of Kuwait.
Limitation
There were some difficulties in this study such as missing data in 2013&2014 because there were lost information’s to report due to break down of Information Technology (IT) system and patient were not available to do PSG (drop out) or left after during the procedure.
Author Contributions: The manuscript was drafted by both authors and was critically reviewed.
Funding: This manuscript received no external funding.
Conflicts of Interest: The authors declare no conflict of interest.
Acknowledgement: The role of Mr. N. Valsala (senior nurse) and Mr. D.Surahnan (senior nurse) at Sleep Disorder Unit, KCMH for their help, support and effort to complete the above work.
References
- Léger D, Poursain B, Neubauer D, et al. An international survey of sleeping problems in the general population. Curr Med Res Opin 24(1), 307-317 (2008).
- Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA 262(11), 1479‑1484 (1989).
- Mellinger GD, Balter MB, Ulenhuth EH. Insomnia and its treatment. Prevalence and correlates. Arch Gen Psychiatry 42(3), 225‑232 (1985).
- Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders: an opportunity for prevention? Jama 262(11), 1479-1484 (1989).
- Breslau N, Roth T, Rosenthal L. Sleep disturbance and psychiatric disorders: A longitudinal epidemiologic study of young adults. Biol Psychiatry 39(6), 411‑418 (1996).
- American Academy of Sleep Medicine International Classification of Sleep Disorders: Diagnostic and Coding Manual. 2nd Edition. Westchester: American Academy of Sleep Medicine (2005).
- Sheau-Hwa Wong. Review of sleep studies of patients with chronic insomnia at a sleep disorder unit. SMJ 56(6), 317-323 (2015).
- Tatineny P, Shafi F, Gohar A. Sleep in the elderly. Mo Med 117(5), 490-495 (2020).
- Mahendran R, Subramaniam M, Chan YH. Psychiatricmorbidity in patients referred to an insomnia clinic. Singapore Med J 48(2), 163-165 (2007).
- Krishnan V, Collop NA. Gender differences in sleep disorders. Curr Opin Pulm Med 12(6), 383-389 (2006).
- Decker AN, Fischer AR, Gunn HE. Socio-Ecological Context of Sleep: Gender Differences and Couples’ Relationships as Exemplars. Curr Psychiatry Rep 24(12), 831-840 (2022).
- Tang J, Liao Y, Kelly BC, et al. Gender and regional differences in sleep quality and insomnia: A general population-based study in Hunan Province of China. Scientific rep 7(1), 43690 (2017).
- Reichner CA. Insomnia and sleep deficiency in pregnancy. Obstet Med 8(4), 168-171 (2015).
- Kundu K, Sharma G, Saini L, et al. Polysomnographic characteristics of the patients having chronic insomnia and obstructive sleep apnea: Evidence for paradoxical insomnia and comorbid insomnia with OSA (COMISA). Indian J. Psychol. Med 44(4), 384-391 (2022).
- Morphy H, Dunn KM, Lewis M, et al. Epidemiology of insomnia: A longitudinal study in a UK population. Sleep 30(3), 274-280 (2007).
- Bhaskar S, Hemavathy D, Prasad S. Prevalence of chronic insomnia in adult patients and its correlation with medical comorbidities. J Family Med Prim Care 5(4), 780 (2016).
- Buysse DJ, Angst J, Gamma A, et al. Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep 31(4), 473-480 (2008).
- Benca RM, Krystal A, Chepke C, Doghramji et al. Recognition and Management of Obstructive Sleep Apnea in Psychiatric Practice. J Clin Psychiatry 84(2), 45191 (2023).
- Khurshid A. Comorbid Insomnia and Psychiatric Disorders-An Update. Innov Clin Neurosci 15(3-4), 28-32 (2018).
[PubMed]
- Johnson EO, Roth T, Breslau N. The association of insomnia with anxiety disorders and depression: exploration of the direction of risk. J Psychiatr Res 40(8), 700-708 (2006).
- Shorr RI, Bauwens SF. Diagnosis and treatment of outpatient insomnia by psychiatric and nonpsychiatric physicians Am J Med 93(1), 78-82 (1992).
 );
More than 60 years old (
);
More than 60 years old ( ).
). 
 ); Circadian Rythem Disorder (
); Circadian Rythem Disorder ( ).
).