Research Article - Neuropsychiatry (2017) Volume 7, Issue 6
"Improvements in Cognitive Function after Continuous Positive Airway Pressure Treatment for Obstructive Sleep Apnea Syndrome"
- Corresponding Author:
- En-Ting Chang
Department of Chest Medicine, Buddhist Tzu Chi General Hospital, Hualien, Taiwan
Tel: +886-3-865-1825
Fax: +886-3-857-7161
Abstract
Abstract
Purpose: Obstructive sleep apnea (OSA) is a sleep disorder characterized by repeated nocturnal desaturation and sleep fragmentation. OSA can result in decreased daytime alertness and neurocognitive dysfunction. Although continuous positive airway pressure (CPAP) has been shown to improve daytime sleepiness in patients with OSA, the effect of CPAP on cognitive function is still controversial.
Methods: A total of 45 patients with OSA were enrolled in this study. All patients completed three cognitive tasks (the psychomotor vigilance task, the Eriksen flanker task and the Stroop task) and two questionnaires (the Pittsburgh Sleep Quality Index (PSQI) and the Epworth Sleepiness Scale (ESS)) to measure cognitive function and daytime sleepiness before and after 3 months of standard CPAP treatment.
Results: The majority of patients showed significant improvements in ESS and PSQI scores after three months of treatment. In addition, CPAP therapy resulted in a decrease in reaction time and error rate in incongruent trials in the flanker task. In the Stroop task, CPAP treatment resulted in an increase in accuracy rate and decreases in error rate and omission rate in congruent trials and an increase in accuracy rate and decreases in reaction time, error rate and omission rate in incongruent trials. There were no significant changes in performance on the psychomotor vigilance task test.
Conclusions: A three-month CPAP therapy resulted in significant improvement in daytime sleepiness and increased executive function but did not have an effect on psychomotor vigilance in patients with OSA.
Keywords
Obstructive sleep apnea, Continuous positive airway pressure therapy, Cognitive function, Flanker task, Stroop task
Introduction
Obstructive sleep apnea (OSA) syndrome involves recurrent upper airway collapses leading to episodes of hypoxemia and arousal during sleep [1]. Clinical features of OSA include snoring, daytime sleepiness, and sleep fragmentation [2]. Many studies have reported that patients with OSA have significant impairments in cognitive function, executive function and psychomotor vigilance [3-5]. Jackson, et al. reported that patients with OSA have significant impairments in attention and vigilance function and also in memory and executive function [6]. These cognitive impairments can lead to difficulty in concentration, increased forgetfulness and problems with decision making.
The treatment of choice for OSA is continuous positive airway pressure (CPAP). CPAP treatment has been shown to correct recurrent upper airway collapses and intermittent hypoxemia, which can in turn decrease sleep fragmentation [7]. Weaver and Chasens [8] and Sanchez, et al. [9] reported that CPAP treatment resulted in partial reversibility of cognitive dysfunction. A metaanalysis conducted by Kylstra, et al. revealed that CPAP treatment for OSA has a minor effect on attention but does not result in significant improvements in vigilance, working memory, memory, verbal fluency or visuoconstruction [10].
Functional magnetic resonance imaging studies have shown that patients with OSA have reduced frontal activation of the anterior cingulate cortices, middle frontal gyri and inferior frontal gyri. Zhang et al found an association between arousal index and severe hypoxia with slow reaction times and frontal mismatch-related activation in patients with OSA, which suggests that both hypoxia and sleep fragmentation contribute to frontal dysfunction in these patients. Structural volume changes have been demonstrated in brain regions in patients with OSA, including areas that regulate memory and executive function (e.g., frontal cortex, anterior cingulate cortex and hippocampus) [11]. In addition, growing evidence suggests that OSA-related changes in brain morphology may improve with CPAP treatment [12]. Two of the most common attentional control paradigms are conflict adaptation and conflict frequency [13]. Attentional control functions are associated with neural activity in the frontal lobe area, particularly in the dorsolateral prefrontal cortex and anterior cingulate cortex.
In this study, we evaluated subjective daytime sleepiness (ESS), sleep quality (PSQI) and three objective clinical tasks (the psychomotor vigilance task, the Eriksen flanker task and the Stroop task) to investigate attention and cognitive functions of patients with OSA before and after 3 months of CPAP treatment.
Methods
In this prospective study, we enrolled 62 patients (47 men and 15 women) with moderate-tosevere OSA (defined as an apnea-hypopnea index (AHI) score ≥15 derived from standard polysomnography) who were treated at the Sleep Center at the Hualien Tzu-Chi General Hospital during the period 1 January 2014 to 31 December 2014. All of the enrolled subjects received CPAP treatment and agreed to participate in follow-up assessments for CPAP compliance. At 3-month follow-up, 45 (33 men and 12 women) of the 62 patients had completed CPAP treatment with good compliance and had undergone the Epworth Sleepiness Scale (ESS), the Pittsburgh Sleep Quality Index (PSQI), the psychomotor vigilance task, the Eriksen flanker task and the Stroop task before and after CPAP treatment. All of the enrolled subjects were >20 years of age. Patients who had previously been diagnosed/treated with any neurological or psychological disease that would have interfered with the accuracy of the five tests were excluded from the study. Those who cannot cooperate with the five tasks were excluded from the study. The hospital’s Institutional Review Board approved this study and all of the participants provided informed consent. The study was funded by Hualien Tzu Chi General Hospital, Taiwan (TCRD 103-34).
▪ Polysomnography and CPAP titration study
All of the patients underwent 1 night of standard type 1 attended polysomnography (Embla A10, Embla, Broomfield, CO) [2] and a CPAP titration study at our Sleep Centre. The optimal CPAP titration pressure was defined as the pressure needed to achieve an AHI of less than 5/hour according to the clinical guidelines for CPAP titration of the American Academy of Sleep Medicine [14]. All of the patients who received CPAP treatment used a US Food and Drug Administration (FDA)-approved CPAP system (Apex medical XT auto CPAP 9S- 005200, Taipei, Taiwan, R.O.C). Compliance for more than 4 hours per day for at least 70% of the 3-month treatment course was defined as good compliance.
Measures
▪ Questionnaires
The ESS is an 8-item questionnaire that asks respondents to answer each question from 0 (not at all likely to fall asleep) to 3 (very likely to fall asleep), with a total score ranging from 0 (minimum) to 24 (maximum) [15]. All of the enrolled subjects also completed the PSQI, a commonly used instrument designed to measure sleep disturbance and sleep habits within a 1 month period [16]. The questionnaire consists of 19 items including subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medications, and daytime dysfunction.
▪ Studied tasks
The enrolled patients were asked to complete psychomotor vigilance; flanker and Stroop tasks, in which all cognitive task were generated using E-prime 2.0.
▪ Psychomotor vigilance task
The patients were instructed to press a button as quickly as possible when a red 50 millisecond (ms)-counter appeared on a small screen. Upon pressing the button, the screen displayed the reaction time for 1 second, thus giving instant feedback on the individual’s performance. Stimuli appeared in a random pattern with an inter-stimulus interval varying between 2 and 10 seconds. Each test lasted for 30 minutes and consisted of approximately 250 stimulus presentations. Each subject also performed a single 1-min practice test before the first trial. We assessed the following outcome measures: (1) reciprocal reaction time (RT) as a measure of speed (1/RT (lapses included) and 1/RT500 (lapses excluded); (2) range between the 10th and 90th percentiles of speed as a measure of variability of response (1/ RT variability, with and without lapses); (3) the fastest 10% of the RTs; (4) the slowest 10% of the RTs; (5) false RTs, defined as the number of false starts divided by the number of valid stimuli in percentage; (6) the number of lapses (defined as a RT>500 ms); (7) average lapse time in milliseconds (defined as the RT during lapses minus 500 ms); and (8) cumulative lapse time in the 30-minute test session [17].
Executive task
▪ Flanker task
In this study, we used the arrow version of the flanker task. Each trial started with a fixed white cross ‘+’ which was displayed on a black background for 500 ms. A horizontal visual array of five arrows appeared immediately after the fixed cross disappeared and lasted for 50 ms. The target arrow was in the centre of the visual array and was flanked on each side by two arrows pointing in the same direction (congruent) or opposite direction (incongruent) as the target. The results of the congruent and incongruent trials were presented as equal probabilities. The patients were required to press a designated key on a keyboard in response to the target arrow as quickly and accurately as possible. The next trial started 2 seconds after a key press or 4 seconds after the presentation of the arrow stimuli of the preceding trial if there was no response. After 12 practice trials, the patients completed four blocks of 64 trials each, with 1-minute breaks between blocks. We assessed the following outcome measures of the congruent and incongruent trials: (1) mean RT of correct trials; (2) intraindividual RT variability of correct trials, defined as the standard deviation of RT divided by the mean RT; (3) accuracy; (4) error rate; (5) omission rate; (6) post-conflict slowing time (slowing after an incongruent, correct trial); and (7) post-error slowing time (slowing after an error) [18].
▪ Color-word stroop task
Subjects were presented with ink colour of colourwords (red, blue, yellow, and green) printed either matched the ink colour, or interfered with it. Congruent and incongruent trials were presented with equal probabilities. Subjects were instructed to respond to the ink color of the words by pressing one of four response keys with maximal speed and accuracy. Each trial started with a fixed cross ‘+’ being displayed for 500 ms, followed by the target. The target was presented until a response was given but did not exceed 2 seconds, and was followed by an inter-trial interval of 2 seconds. After 12 practice trials, the patients completed four blocks of 72 trials each, with 1 minute breaks between blocks. We assessed the following outcome measures of the congruent and incongruent trials: (1) mean RT of correct trials; (2) intra-individual RT variability of correct trials, defined as the standard deviation of RT divided by the mean RT; (3) accuracy; (4) error rate; (5) omission rate; (6) post-conflict slowing time (slowing after an incongruent, correct trial); and (7) post-error slowing time (slowing after an error) [19].
Data collection
Data including age, sex, body mass index, daytime sleepiness (determined using the ESS and PSQI) were recorded. All of the study participants completed the psychomotor vigilance, flanker and Stroop tasks in a quiet isolation room in the morning without any interference. The questionnaires and tasks were performed at baseline (before treatment) and at 3 months after CPAP treatments.
Statistical analysis
The sample size was determined according to previous studies on CPAP treatment in patients with anxiety and depression [10]. The paired t-test was used to compare scores on the ESS, PSQI, and PVT, flanker and Stroop tasks before and after CPAP treatment. A p value<0.05 was considered to indicate statistical significance. All statistical analyses were performed using the statistical package SPSS for Windows (Version 14.0, SPSS, Chicago, IL).
Results
▪ Demographic data
Of the 62 enrolled patients with OSA, 45 (33 men, 12 women) had good compliance with CPAP treatment and completed all of the tasks. The mean age of these patients was 47.8 ± 10.7 years, the mean body mass index was 29.8 ± 4.6 kg/m2 and mean neck circumference was 39.0 cm. The majority (93%,43/45) of the enrolled patients or their partners complained about snoring. The mean AHI was 57.9 ± 25.4/hour and the mean oxygen desaturation index was 42.3 ± 25.8/hour (Table 1). Between 62 enrolled subjects, 10 patients cannot cooperate with our CPAP machine with poor compliance and 7 patients did not want second task due to long task time. In the other hands, only 15 patients had comorbid medical disease with diabetes mellitus and hypertension. Those who had comorbidity with OSA continued their usual drugs through our 3-month study period.
| Subject n | 45 (males=33, females=12) |
|---|---|
| Age (years) | 47.778 ± 10.693 |
| BMI (kg/ m²) | 29.841 ± 4.555 |
| NC (cm) | 38.955 ± 3.571 |
| AHI (/h) | 57.944 ± 25.417 |
| ODI (/h) | 42.284 ± 25.800 |
| AI (/h) | 31.630 ± 17.706 |
| NREM sleep (%) | |
| N1 | 29.347 ± 14.780 |
| N2 | 42.401 ± 13.533 |
| N3 | 7.281 ± 6.829 |
| REM sleep (%) | 26.851 ± 40.801 |
| Total sleep time (min) | 389.307 ± 41.133 |
| Sleep effect (%) | 87.588 ± 6.755 |
Table 1: Demographic and polysomnographic data.
▪ ESS and PSQI questionnaires
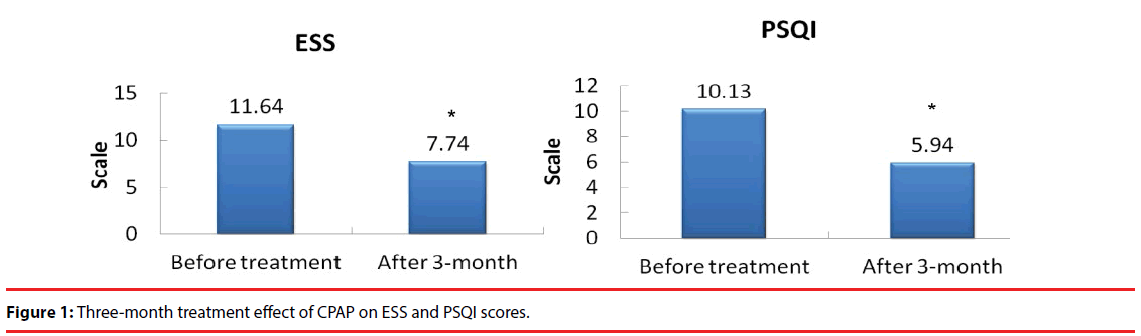
Before CPAP treatment, the mean ESS score was 11.6 and the mean PSQI was 10.1. After 3 months of CPAP treatment, there were significant decreases in ESS score and PSQI, indicating improvements in subjective daytime sleepiness and sleep quality (Figure 1).
▪ Psychomotor vigilance task (PVT)
In the present study, no significant improvement in PVT was noted after three months of CPAP therapy (Table 2).
| PVT measures | Baseline | CPAP treatment |
|---|---|---|
| 1/RT (1/s) | 3.38 ± .69 | 3.27 ± .65 |
| False RT (number >100 ms) | .016 ± .13 | .016 ± .13 |
| Lapses | 15.76 ± 40.00 | 5.69 ± 13.56 |
| Average Lapse Time | 251.12 ± 242.49 | 167.32 ± 158.10 |
| Total Lapse Time (s) | 2.09 ± 3.56 | 1.24 ± 1.43 |
Table 2: Three-month treatment effect of CPAP on the psychomotor vigilance task.
Executive Task
▪ Flanker task
No significant improvements were found in reaction time, accuracy rate, error rate or omission rate in congruent trials in the flanker task after 3 months of CPAP treatment. A significantly shorter reaction time (p=0.02) and lower error rate (p<0.001) were found in the incongruent trials in the flanker task after 3 months of CPAP therapy. There were no significant changes in post-conflict slowing or post-error slowing in the flanker task after CPAP treatment (Table 3).
| Flanker task measures | Baseline | CPAP treatment |
|---|---|---|
| Congruent trials | ||
| Correct RT | 383.44 ± 111.88 | 364.58 ± 83.42 |
| AR (%) | 96.72 ± 5.68 | 97.96 ± 6.30 |
| ER (%) | 0.64 ± 1.80 | 0.21 ± 0.42 |
| OR (%) | 2.63 ± 5.03 | 1.83 ± 6.13 |
| Incongruent trials | ||
| Correct RT | 482.06 ± 171.80 | 437.69 ± 80.69* |
| AR (%) | 88.04 ± 16.30 | 93.14 ± 8.68 |
| ER (%) | 7.23 ± 7.65 | 5.08 ± 6.14** |
| OR (%) | 4.73 ± 14.36 | 1.77 ± 5.84 |
| Post-conflict slowing | 8.65 ± 16.80 | -0.53 ± 30.48 |
| Post-error slowing | -24.22 ± 182.94 | -18.07 ± 167.67 |
Table 3: Three-month treatment effect of CPAP on the flanker task.
▪ Stroop task
In the Stroop task, a significantly increased accuracy rate (p=0.006) and significantly decreased error (p=0.007) and omission (p=0.048) rates in congruent trials were found after 3 months of CPAP therapy. In addition, a significantly shorter reaction time (p=0.005), higher accuracy rate (p<0.001), lower error rate (p<0.001) and lower omissions rate (p<0.001) were also noted in the incongruent trials of the Stroop task after 3 months of CPAP therapy.
However, no significant changes in postconflicting and post-error slowing were noted (Table 4).
| Stroop task measures | Baseline | 3 months after CPAP treatment |
|---|---|---|
| Congruent trials | ||
| Correct RT | 693.58 ± 144.86 | 657.09 ± 149.60 |
| AR (%) | 87.95 ± 17.91 | 95.99 ± 6.29** |
| ER (%) | 6.45 ± 10.55 | 2.29 ± 3.49** |
| OR (%) | 5.60 ± 13.10 | 1.72 ± 4.93* |
| Incongruent trials | ||
| Correct RT | 845.89 ± 168.41 | 779.36 ± 161.89* |
| AR (%) | 80.00 ± 21.03 | 91.37 ± 9.17** |
| ER (%) | 12.65 ± 13.70 | 6.35 ± 6.76** |
| OR (%) | 7.35 ± 13.05 | 2.28 ± 5.62** |
| Post-conflict slowing | 20.37 ± 45.30 | -4.04 ± 69.40 |
| Post-error slowing | 55.65 ± 74.23 | 78.56 ± 93.25 |
Table 4: Three-month treatment effect of CPAP on color-word Stroop task.
Discussion
In the present study, a three-month regimen of CPAP therapy resulted in significant improvements in daytime sleepiness and executive function, especially in incongruent trials.
Daytime sleepiness is the chief complaint of patients with OSA. The ESS and PSQI are the two most commonly used self-reported clinical evaluation tools in sleep laboratories, and their scores have been shown to improve after four weeks of CPAP treatment [20]. Deng reported that 3 months of CPAP therapy resulted in improved ESS and PSQI scores in patients with OSA, which is consistent with our findings [21].
Vigilance and attentional control have been shown to be impaired in patients with OSA. Thomann reported that patients with OSA had a slower speed, greater variability, more lapses, and longer lapse times in psychomotor vigilance tasks than healthy controls [22]. Furthermore, Verstraeten, et al. reported that patients with OSA showed decreases in visual vigilance, characterized by lapses in attention and state instability [4]. However, the treatment effect of CPAP in patients with OSA has rarely been studied. In a meta-analysis, Kylstra, et al. found that CPAP had a significant effect on divided attention but a weak effect on improving sustained attention [10]. On the other hand, Aloia, et al. reported no improvement in constructional ability or psychomotor function after CPAP therapy [23]. Persistent intrinsic neural dysfunction may explain the functional impairments in patients with OSA. Our study also showed that three months of CPAP therapy did not result in improvement in psychomotor vigilance tasks (sustained attention).
The flanker task is a clinical cognitive evaluation tool designed to assess conflict adaptation. Tulek, et al. reported that the degree of conflict adaptation was markedly lower in patients with OSA than in healthy controls [13]. In the present study, there were no significant improvements in the congruent trials; however, significant improvements in the incongruent trials including decreased reaction time, error rate and omission rate were noted after 3 months of CPAP therapy. In addition, there were no significant changes in post-conflict slowing and post-error slowing in the flanker task after CPAP treatment. The Stroop task is used to measure the effect of conflict frequency using colored words. Two blocks of the Stroop task were congruent and two incongruent trials. Although Tulek, et al. reported no significant differences in reaction time in the congruent and incongruent Stroop tasks between patients with OSA and controls, we found that CPAP resulted in an increase in accuracy rate and decreases in error rate and omission rate in the congruent trials, as well as a decrease in response time, error rate, and omission time and an increase in accuracy rate in the incongruent trials. In neuroimaging studies, both flanker and Stroop tasks have been shown to be affected by the anterior cingulate cortex [24,25], with diminished regional and often unilateral grey matter loss in brain morphology in patients with OSA [26]. However, Prilipko, et al. reported that CPAP treatment for patients with OSA did not result in complete recovery from the hypoxemic insults in the left and right insula, right medial prefrontal cortex, and right anterior cingulate cortex. This implies that some of the hypoxemic damage in patients with OSA cannot be reversed, even with long-term CPAP therapy [27].
There are several limitations to this study. First, we did not perform the same cognitive tasks in healthy controls for comparison. Therefore, practice effect of the measuring cognitive task should be taken into consideration. However, practice effect was seldom seen in Stroop and Flanker task [28], and improvements about 3-9% was described as large and clinical relevant other than practice effect [29]. (The major improvements of Flanker and Stroop task in our study were greater than 10%). Second, we did not include a randomized control group with sham CPAP. Third, the patient number was relatively small. Further large-scale studies are needed to confirm our results.
In conclusion, we found that a three-month regimen of CPAP therapy resulted in significant improvement in daytime sleepiness and executive function but not in psychomotor vigilance, particularly in the incongruent trials in patients with OSA. This finding suggests that CPAP therapy has a greater effect on conflict adaptation than on psychomotor attention.
Funding
Buddist Tzu Chi General Hospital provided financial support in the form of funding for design and data acquisition. The sponsor had no role in the design or conduct of this research.
Conflict of Interest
All authors certify that they have no affiliations with or involvement in any organisation or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership or other equity interest; and expert testimony or patentlicencing arrangements) or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Acknowledgement
Dr. Chang handled all of the projects including data collection, program script, data analysis and script writing. Mrs Li collected the data, cognitive data analysis and script initial writing. Dr. Shen collects data and data analysis, as well as script writing. Miss Wang collected polysomnographic data. And, Mr. Jan has written the program for computer task.
References
- Young T, Palta M, Dempsey J, et al. The occurrence of sleep-disordered breathing among middle-aged adults. N. Engl. J. Med 328(17), 1230-1235 (1993).
- The American Academy of Sleep Medicine Task Force. Sleep-related breathing disorders in adults: recommendations for syndrome definition, measurement techniques in clinical research. Sleep 22(5), 667-689 (1999).
- Lal C, Strange C, Bachman D. Neurocognitive impairment in obstructive sleep apnea. Chest 141(6), 1601-1610 (2012).
- Verstraeten E, Cluydts R, Pevernagie D, et al. Executive function in sleep apnea: controlling for attentional capacity in assessing executive attention. Sleep 27(4), 685-693 (2004).
- Battol-Anwar S, Kales SN, Patel SR, et al. Obstructive sleep apnea and psychomotor vigilance task performance. Nat. Sci. Sleep 6(1), 65-71 (2014).
- Jackson ML, Howard MD, Barnes M. Cognition and daytime functioning in sleep-related breathing disorders. Prog. Brain. Res 190(1), 53-68 (2011).
- Lamphere J, Roehrs T, Zorick F, Conway W, Roth T. Recovery of alertness after CPAP in apnea. Chest 96(6), 1364-1367 (1989).
- Weaver TE, Chasens ER. Continuous positive airway pressure treatment for sleep apnea in older adults. Sleep. Med. Rev 11(2), 99-111 (2007).
- Sanchez AI, Martinez P, Miro E, et al. CPAP and behavioral therapies in patients with obstructive sleep apnea: effects on daytime sleepiness, mood and cognitive function. Sleep. Med. Rev 13(3), 223-233 (2009).
- Kylstra WA, Aaronson JA, Hofman WF, et al. Neuropsychological functioning after CPAP treatment in obstructive sleep apnea: A meta-analysis. Sleep. Med. Rev 17(5), 341-347 (2013).
- Zhang X, Ma L, Li S, et al. A functional MRI evaluation of frontal dysfunction in patients with severe obstructive sleep apnea. Sleep. Med 12(4), 335-340 (2011).
- Ferini-Strambi L, Marelli S, Galbiati A, et al. Effects of continuous positive airway pressure on cognition and neuroimaging data in sleep apnea. Int. J. Psychophysiol 89(2), 203-212 (2013).
- Tulek B, Atalay NB, Kanat F, et al. Attentional control is partially impaired in obstructive sleep apnea syndrome. J. Sleep. Res 22(4), 422-429 (2013).
- Kushida CA, Chediak A, Berry RB, et al. Clinical Guidelines for the Manual Titration of Positive Airway Pressure in OSA Patients Published in the Journal of Clinical Sleep Medicine. J. Clin. Sleep. Med 4(2), 157-171 (2008).
- Johns MW. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep 14(6), 540–545 (1991).
- Buysse DJ, Reynolds CF, Monk TH, et al. The Pittsburgh Sleep Quality Index (PSQI): A new instrument for psychiatric research and practice. Psychiatry. Res 28(2), 193-213 (1989).
- Dinges DF, Powell JW. Microcomputer analyses of performance on a portable, simple visual RT task during sustained operations. Behav. Res. Methods. Instrum. Comput 17(6), 652-655 (1985).
- Eriksen BA, Eriksen CW. Effects of noise letters upon identification of a target letter in a non-search task. Percept. Psychophy 16(1), 143-149 (1974).
- Macleod CM. Half a century of research on the Stroop effect: an integrative review. Psychol. Bull 109(2), 163-203 (1991).
- Skomro RP, Gjevre J, Reid J, et al. Outcomes of home-based diagnosis and treatment of obstructive sleep apnea. Chest 138(2), 257-263 (2010).
- Deng T, Wang Y, Sun M, et al. Stage-matched intervention for adherence to CPAP in patients with obstructive sleep apnea: a randomized controlled trial. Sleep. Breath 17(2), 791-801 (2012).
- Thomann J, Baumann CR, Landolt HP, et al. Psychomotor vigilance task demonstrates impaired vigilance in disorders with excessive daytime sleepiness. J. Clin. Sleep. Med 10(9), 1019-1024 (2014).
- Aloia MS, Arnedt JT, Davis JD, et al. Neuropsychological sequelae of obstructive sleep apnea-hypopnea syndrome: a critical review. J. Int. Neuropsychol. Soc 10(5), 772-785 (2004).
- Botvinick MM, Cohen JD, Carter CS. Conflict monitoring and the anterior cingulate cortex: an update. Trends. Cogn. Sci 8(12), 539-546 (2004).
- Pardo JV, Pardo PJ, Janer KW, et al. The anterior cingulate cortex mediates processing selection in the Stroop attentional conflict paradigm. Proc. Natl. Acad. Sci. U S A 87(1), 256-259 (1990).
- Macey PM, Henderson LA, Macey KE, et al. Brain morphology associated with obstructive sleep apnea. Am. J. Respir. Crit Care. Med 166(10), 1382-1387 (2002).
- Prilipko O, Huynh N, Thomason ME, et al. An fMRI study of cerebrovascular reactivity and perfusion in obstructive sleep apnea patients before and after CPAP treatment. Sleep. Med 15(8), 892-898 (2014).
- Chen A, Tang D, Chen X. Training reveals the sources of Stroop and Flanker interference effects. Plos. One 8(10), e76580 (2013).
- Wesnes K, Pincock C. Practice effects on cognitive task: a major problem? Lancet. Neurol 1(8), 473 (2002).