Research Article - (2022) Volume 12, Issue 1
Cross sectional epidemiological study of Obstructive Sleep Apnoea (OSA) among inpatient with severe mental illness at long term rehab wards in Kuwait.
Mohamed Binali1, Hammad Mahmoud2*, Mohamed Abuzeid3
1Department of Psychology, Mental Disorders unit, Sabah medical area, Kuwait, Saudi Arabia
2Department of Psychiatry, Sleep disorder Unit, Kuwait centre for mental health, Kuwait, Saudi Arabia
3Department of Psychiatry, Arab Open University in Kuwait, Sabah medical area, Kuwait, Saudi Arabia
*Corresponding Author:Hammad Mahmoud
Department of Psychiatry, Sleep disorder Unit, Kuwait centre for mental health, Kuwait, Saudi Arabia
E-mail:[email protected].
Received date: 27-Dec-2022, Manuscript No. NPY-21-39853;
Editor assigned date: 29-Dec-2022, PreQC No. NPY-21-39853(PQ);
Reviewed date: 08-Jan-2022, QC No NPY-21-39853;
Revised date: 19-Jan-2022, Manuscript No. NPY-21-39853(R);
Published date: 26-Jan-2022, DOI: 10.37532/1758-2008.2022.12(1).616
Abstract
Individuals with schizophrenia are 2 times-3 times more likely to die at an early age because of cardiovascular, metabolic, and infectious diseases. Although sleep disturbances are not included in the diagnostic criteria for schizophrenia, they are consistently reported in those patients. A high prevalence of Obstructive Sleep Apnea (OSA) is reported in patients with schizophrenia. Both genetically determined and medication-induced obesity can lead to OSA,” Schizophrenic patients who have OSA generally have worse outcomes, worse quality of life, higher mortality, and more severe symptoms. Methods: A cross sectional epidemiological study for a total number of 36 patients diagnosed with severe mental illness, 20 females and 16 males, chosen from two rehab wards of the long stay inpatient unite at Kuwait Centre for Mental Health. KCMH diagnosed as (Schizophrenia, Schizoaffective and Bipolar Disorder), with the aim of identifying and screening OSA. Results: By using stop bang scale, 18 patients (50%) had a score of 1, indicate mild risk of apnoea-12 patients (33.3%) had a score of 2 indicate moderate risk of apnea, and 6 patients (16.7 %) has score of 3 indicate high risk of apnea. Four patients out of 36 have normal body weight (11.1%), 7 out of 36 have overweight (19.4%), 25 have obesity (69.4%). Regarding waist size more than 38 cm was in 29 patients (80%), indicating increase in developing truncal obesity. Conclusion: Stop bang is a brief, easy-to-use screening tool for OSA in individuals with severe mental illness. There is a high prevalence of OSA symptoms among in patients with schizophrenia in long stay rehab wards. Primary prevention of OSA by targeting obesity may be the most effective strategy to reduce OSA among individuals with severe mental illness.
Keywords
Schizophrenia, obstructive sleep apnea, stop bang scale, rehab wards
Introduction
Schizophrenia is a severe psychiatric disorder that affects less than 1% of the population worldwide, and represents an immense burden for the patients and the entire society. It commonly starts earlier among men, and is linked with considerable disability where it could seriously affect educational and occupational performance [1]. People with schizophrenia are 2 times-3 times more likely to die at an early age in comparison to the general population. This is associated to physical illnesses, such as cardiovascular, metabolic, and infectious diseases [2].
Difficulties initiating or maintaining sleep are frequently encountered in patients with schizophrenia. Disturbed sleeps are found in 30%-80% of schizophrenic patients, depending on the degree of psychotic symptomatology. Measured by polysomnography, reduced sleep efficiency and total sleep time, as well as increased sleep latency, are founded in most patients with schizophrenia and appear to be an important part of the pathophysiology of this disorder. Some studies also reported alterations of stage 2 sleep, Slow Wave Sleep (SWS) and Rapid Eye Movement (REM) sleep variables, i.e. reduced REM latency and REM density [3].
A number of sleep parameters, such as the amount of SWS and the REM latency, are significantly correlated to clinical variables, including severity of illness, positive symptoms, negative symptoms, outcome, neurocognitive impairment and brain structure [4].
Although sleep disturbances are not included in the diagnostic criteria for schizophrenia, they are consistently reported in those patients. Similarly, while research in schizophrenia has primarily and traditionally focused on waking-related abnormalities, sleep has been increasingly studied in schizophrenia populations and consistently found to be disturbed [5].
Schizophrenia and sleep disturbances are both associated with a higher risk for health problems. Compared with patients with either condition alone, patients who have both disorders generally have worse outcomes and quality of life, higher mortality, and more severe symptoms [6].
In addition, sleep disorders affect social and cognitive functioning, and therefore are likely to contribute in a significant way to the daily challenges commonly experienced by patients with schizophrenia [7].
Obstructive Sleep Apnoea Syndrome (OSAS) is considered one of the most significant sleep disorders, with a prevalence of 9%-17%. It is a chronic respiratory condition, in which the airflow is repeatedly blocked during sleep, resulting in recurrent hypoxia, hypercapnia, and frequent arousal. What is amazingly disturbing, the fact: up to one billion middle-aged people have OSAS worldwide, and the number of OSAS patients has tended to increase along with the obesity epidemic. OSAS which is not classified as Metabolic Syndrome (MetS) components may nevertheless exacerbate cardiovascular disease in MetS patients [8].
Various studies have reported a high prevalence of OSA in patients with schizophrenia -15.4% in one meta-analysis, for example, and 14% in a study of 175 outpatients. Another study with a meta-analysis reporting an OSA prevalence of 15.4% in schizophrenic patients [9].
Obesity may be one factor underlying this connection. “Excessive weight gain is a common side effect of APs, and both genetically determined and medication-induced obesity can lead to OSA,” are according to the review [10].
One study in patients with severe mental illness treated at a primary care clinic found that 69% had high scores for the Stop-Bang (a screening questionnaire for OSA), and among this group 62% had a diagnosis of schizophrenia [11].
Another study found that among schizophrenia patients referred to a sleep clinic while hospitalized in a psychiatric inpatient unit, nearly half-met criteria for OSA [12]. Age, gender, Body Mass Index (BMI), and chronic neuroleptic use all have a significant independent effect on the presence of OSA in psychiatric patients, with the schizophrenic group having significantly higher BMI and increased rates of sleep apnoea [13].
In addition, Obesity is a likely factor responsible for the association between schizophrenia and OSA. Excessive weight gain is a common side effect of psychotropic medications, and both genetically determined and medication-induced obesity can lead to OSA. In addition to Antipsychotic medications related weight gain, schizophrenia patients have poorer physical health than the general population due to sedentary life style heavy smocking and comorbid subs abuse.
In one study of 175 outpatients with schizophrenia, a high prevalence of OSA (14%) was observed. BMI was found to be significantly higher in those patients diagnosed with OSA when compared with those without an OSA diagnosis [14]. Another study investigated an elderly schizophrenia group (N=44), since the prevalence of sleep-disordered breathing tends to increase with age. 85% of these patients had 10 respiratory events per hour of sleep and reported more daytime sleepiness compared to a small group (N=8) of seasonal affective disorder patients, although these symptoms were unrelated to their BMI [15].
Now it is clear that sleep dysfunction is an important aspect of schizophrenia, and for some patients, even sleep abnormalities may meet diagnostic criteria for a sleep disorder. Indeed, increased rates of OSA, Restless Leg Syndrome (RLS), Periodic Limb Movement Disorder (PLMD), and Circadian Rhythm Dysfunction (CRD) have been observed in schizophrenia patients [16].
Another thing reported among researchers was the worsening of the psychotic symptoms with sleep disturbances among the schizophrenic population, where several studies have found associations between sleep disturbances and symptom severity [17]. In one study of adolescents at ultra-high risk for psychosis, those who displayed poorer sleep quality, as determined by increased wake time after sleep onset, more movements during sleep, and decreased sleep efficiency, had worsening positive symptoms after 12 months [18]. It was always thought, Insomnia is heralding sign of impending psychosis, whereas fragmented circadian rhythms in individuals at CHR for psychosis were associated with more severe psychotic symptoms [19].
Among patients diagnosed with schizophrenia, those with positive symptoms tend to have more disrupted sleep–wake patterns and worse quality of sleep [20]. While those more compliant with APs treatment are less symptomatic [21].
Objective and subjective sleep quality and efficiency can also predict next-day symptom severity, including increased auditory hallucinations, paranoia, and delusions in chronic patients with schizophrenia [22]. Moreover, a study showed that schizophrenia patients with sleep disturbances and weaker circadian rhythms had worse performance in neuropsychological tests. Abnormalities in sleep-specific EEG patterns are also related to selective deficits in learning and memory in schizophrenia. For example, a study showed a correlation between the reduction in SWS and lower scores in a visuo spatial memory test in chronic patients with schizophrenia, which underlines an important role of SWS in memory consolidation [23].
There is also evidence that psychotic symptoms can lead to sleep disturbances. Specifically, psychotic experiences interfere with the ability to sleep well, and resulting sleep problems lead to daytime tiredness, thus impairing the ability of schizophrenia patients to cope with their psychotic symptoms [24].
All subjects in these study were taken from two wards in the long stay unite at Kuwait Centre for Mental Health. It is the only psychiatric facility with inpatient wards in the state of Kuwait, it holds more than 600 bed and has 5 days a week outpatient clinic that accept more than 300 patients daily. It has 80 beds distributed in five wards for the long stay patients where they receive medication& psychosocial rehabilitation under the supervision of two consultant psychiatrists and two psychiatric registrars; in addition to a day care unite that follow up the long stay ward’s discharged patients to continue their rehabilitation recovery program in the community.
Methods
Study design
It is a cross sectional epidemiological study for long stay inpatient at rehab wards in the Kuwait Centre for mental illness for identifying and screening of obstructive sleep apnoea.
In this study, our selection includes patients diagnosed with psychiatric disorder according to DSM V and has medical comorbidities such as COPD, Obesity, CVD and others.
Study setting and location
The study conducted at Kuwait centre for mental health. It is the only centre located at Sabah medical area in the state of Kuwait. There were two rehab wards involved in the study.
Study Population
The population samples were drawn from: two long stay rehab wards for inpatient with severe mental illness such as schizophrenia, Schizoaffective and Bipolar Disorder. All aspects of participant selection were based on having severe mental illness, being on psychotropic medication, and having medical comorbidities.
The total number were 36 patients, 20 females and 16 males, (females’ numbers are more than males in the sample that were chosen). There were Inclusion criteria: age from 18-65 years old, severe mental disorder according to DSM V, medical issues, and on psychotropic medications. There were also Exclusion criteria: individual using substance or diagnosed personality disorders. This is used to set a standard for the patients to involve in the study and ensure their safety.
They were screened with Stop Bang and Epworth questioners by two psychiatrists, senior registrar allocated by the research team who were not involve with the care and treatment of the patients. Prior to the study, consent was taken from each patient.
Data
It was collected by two researchers and nurses and was analysed by SPSS version 26. We used descriptive statistics and analysis methods such as frequency tables and bar chart to describe the association between different independent variables such as gender, age, BMI, waist and neck circumstances, stop bang and Epworth questioners.
Results
The independent variables as shown in Table 1, are total number is 36 patients, the mean age was 49.1 years, the mean BMI was 2.58, the mean neck size was 14.5 cm, and mean waist size was 42.7 cm (Table 1).
Table 1: The independent variables are shown as descriptive statistics.
| Descriptive statistics | |||||
|---|---|---|---|---|---|
| N | Minimum | Maximum | Mean | Std. Deviation | |
| Patient name | 36 | 1.00 | 36.00 | 18.5000 | 10.53565 |
| Gender | 36 | 1.00 | 2.00 | 1.5556 | .50395 |
| Patient age | 36 | 27.00 | 68.00 | 49.1389 | 10.81309 |
| Body mass index | 36 | 1 | 3 | 2.58 | .692 |
| Neck size | 36 | 11.00 | 18.00 | 14.5278 | 1.68160 |
| Waist size | 36 | 31.00 | 53.00 | 42.6667 | 5.37720 |
| Epworth scale score | 36 | 1.00 | 3.00 | 1.2500 | .60356 |
| Stopbang scale sore | 36 | 1.00 | 3.00 | 1.6667 | .75593 |
| Smoking cigarette | 36 | 1.00 | 2.00 | 1.7500 | .43916 |
| Valid N (listwise) | 36 | ||||
Looking at Table 2, female numbers are 20 (55.6%) and male number are 16 (44.4%) from two different wards (Table 2).
Table 2: There are two different wards of Male and Female number of people
| Gender | |||||
|---|---|---|---|---|---|
| Frequency | Percent | Valid percent | Cumulative percent | ||
| Valid | Male | 16 | 44.4 | 44.4 | 44.4 |
| Female | 20 | 55.6 | 55.6 | 100.0 | |
| Total | 36 | 100.0 | 100.0 | ||
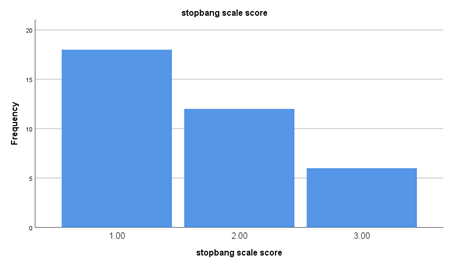
In Figure 1, Stop bang scale score showed: there were 18 patients who score 1, 12 patients score 2 and 6 patients score 3. (Score 1 indicate low risk of OSA, score 2 indicate intermediate risk of OSA, 3 indicate high risk of OSA) (Figure 1).
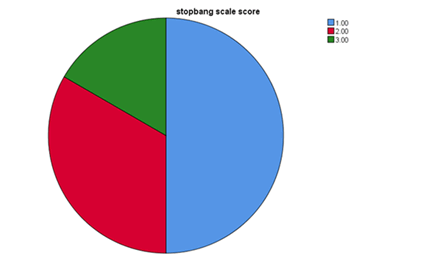
In the Table 3, the stop bang scale score showed: 18 patients out of 36 have a score of 1 (50%), indicate mild risk of apnoea, 12 patients out of 36( 33.3%) have score of 2 indicate moderate risk of apnoea; and 6 patients out of 36 have score of 3( 16.7%) indicate high risk of apnoea . It showed also 50% of rehab patients have moderate to high risk of apnoea (also showed in Pie chart 1) (Table 3).
Table 3: The Stop Bang Scale Score showed, also 50 % of rehab patients have moderate to high risk of apnoea
| Stop bang scale score | |||||
|---|---|---|---|---|---|
| Frequency | Percent | Valid percent | Cumulative percent | ||
| Valid | 1 | 18 | 50.0 | 50.0 | 50.0 |
| 2 | 12 | 33.3 | 33.3 | 83.3 | |
| 3 | 6 | 16.7 | 16.7 | 100.0 | |
| Total | 36 | 100.0 | 100.0 | ||
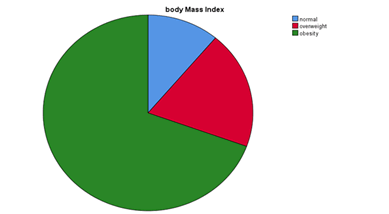
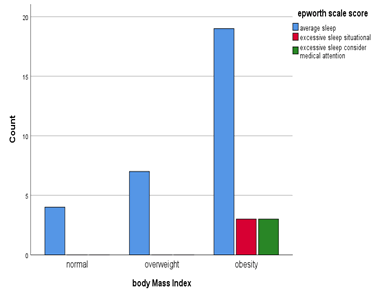
Table 4 shows Body Mass Index (BMI) score results. There were 4 patients out of 36 have normal body weight (11.1%), 7 patients out of 36 were overweight; (19.4%), 25 patients out of 36 have obesity (69.4%). It showed t about 2/3 of the sample were obese (also shown in the Pie chart 2) (Table 4).
Table 4: Results of Body Mass Index (BMI).
| Body mass index | |||||
|---|---|---|---|---|---|
| Frequency | Percent | Valid percent | Cumulative percent | ||
| Valid | Normal | 4 | 11.1 | 11.1 | 11.1 |
| Overweight | 7 | 19.4 | 19.4 | 30.6 | |
| Obesity | 25 | 69.4 | 69.4 | 100.0 | |
| Total | 36 | 100.0 | 100.0 | ||
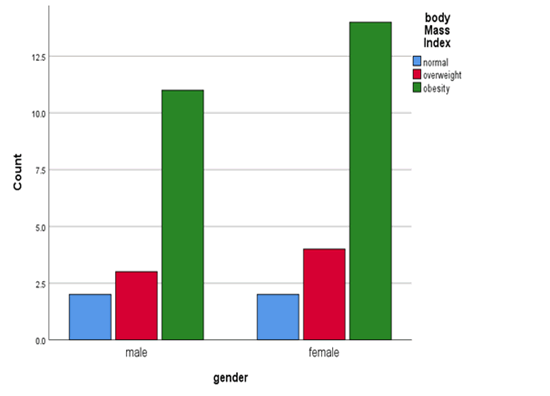
In Figure 2 regarding the gender difference and BMI score, it showed females has higher numbers of obese and overweight patients and difference between both genders are not significant. It showed a normal BMI for both were equal (Figure 2).
In Table 5, Regarding patients waist size, there are 29 patients out of 36 (80%) who waist size were more than 38 cm, indicating increase in developing Truncal obesity (Table 5, Figure 3).
Table 5: Regarding patient’s waist size indicating increase in developing Truncal obesity.
| Waist Size | |||||
|---|---|---|---|---|---|
| Frequency | Percent | Valid Percent | Cumulative Percent | ||
| Valid | 31.00 | 1 | 2.8 | 2.8 | 2.8 |
| 33.00 | 1 | 2.8 | 2.8 | 5.6 | |
| 35.00 | 1 | 2.8 | 2.8 | 8.3 | |
| 36.00 | 1 | 2.8 | 2.8 | 11.1 | |
| 37.00 | 3 | 8.3 | 8.3 | 19.4 | |
| 39.00 | 3 | 8.3 | 8.3 | 27.8 | |
| 40.00 | 2 | 5.6 | 5.6 | 33.3 | |
| 41.00 | 5 | 13.9 | 13.9 | 47.2 | |
| 42.00 | 1 | 2.8 | 2.8 | 50.0 | |
| 43.00 | 3 | 8.3 | 8.3 | 58.3 | |
| 44.00 | 1 | 2.8 | 2.8 | 61.1 | |
| 45.00 | 4 | 11.1 | 11.1 | 72.2 | |
| 46.00 | 1 | 2.8 | 2.8 | 75.0 | |
| 47.00 | 3 | 8.3 | 8.3 | 83.3 | |
| 50.00 | 2 | 5.6 | 5.6 | 88.9 | |
| 51.00 | 3 | 8.3 | 8.3 | 97.2 | |
| 53.00 | 1 | 2.8 | 2.8 | 100.0 | |
| Total | 36 | 100.0 | 100.0 | ||
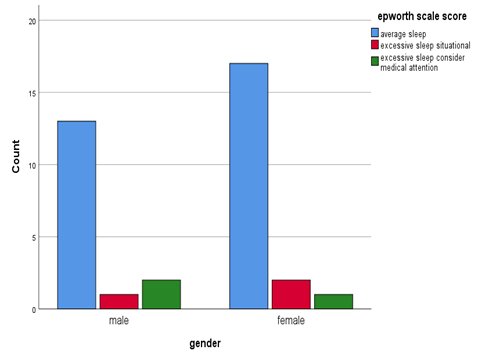
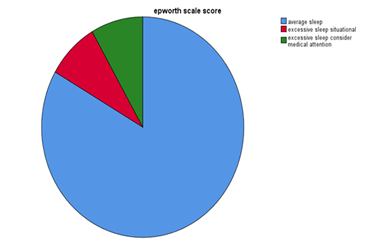
In above Figure 3, the average sleep Epworth scale score within female population was 17 out of 20 more than male population that was 13 out of 16 and excessive sleep situational score was 2 out of 20 for female and 1 out of 16 for male. But excessive sleep considers medical attention was 2 out of 16 for male and 1 out of 20 for female (as shown in the table and Pie chart 3) (Table 6).
Table 6: The excessive sleep consider medical attention of female population.
| Frequency | Percent | Valid percent | Cumulative percent | ||
|---|---|---|---|---|---|
| Valid | Average sleep | 30 | 83.3 | 83.3 | 83.3 |
| Excessive sleep situational | 3 | 8.3 | 8.3 | 91.7 | |
| Excessive sleep consider medical attention | 3 | 8.3 | 8.3 | 100.0 | |
| Total | 36 | 100.0 | 100.0 | ||
Figure 4 showed there are 6 patients who are obese and score 3 on stop bang scale , there are 10 obese patients who score 1 on stop bang scale and there are 9 patients who were obese and score 2 on stop bang scale .
The Figure 5 showed for stop bang scale score of 1(low risk of OSA), there were 18 patients out of 36 (50% had low risk). With stop bang score 2 and 3 (moderate and sever risk of OSA), There were 18 out of 36 (50%) and 25 patients out of 36 are obese (69.4%).
In Figure 6, the number of obese patients were 25, 19 has average sleep score, 6 has excessive sleep (3 need medical attention). There are overweight 7 patients and 4 patients with normal weight.
Limitations
Sample size was small. There are lacks of awareness about OSA in the community and among professional. Patient self-report of OSA was used to calculate the Stop bang score; however, this was verified by nurse reporting.
Though there is a significant association of STOP Bang scores with an OSA diagnosis, we were not able to us polysomnography on the above sample in this stage of research.
Discussion
OSA is observed in a greater proportion of schizophrenia patients compared to the general population. Furthermore, weight gain is the strongest link to OSA, with several APs leading to unwanted weight gain. It is important to highlight that many studies suggest that those at risk for OSA may go unnoticed, and so it may be beneficial to implement screening for OSA and related sleep disorders more widely [25].
The thing that made us study a group of 36 patients in 2 long stay wards, 20 females and 16 males (age from 18-65 years, with severe mental disorder) in Kuwait Center for Mental Health (KCMH), searching for undiagnosed OSA among them.
Overall Very little data has been obtained, there were insufficient reports on the prevalence of OSA in schizophrenia and other psychotic disorders, to draw conclusions about the prevalence of OSA in this group. Several studies made on small groups of patients show that it can be as high as 15% to 48% [26].
The first goal of the study in hand was to determine if there are elevated levels of OSA in individuals with severe chronic mental disorders in the long stay wards of KCMH.
In the sample studied, we demonstrated a very high prevalence of sleep apnea. Comorbidities and especially obesity were more prevalent in patients with coexisting schizophrenia and OSA in comparison to schizophrenia with no OSA patients.
In our study and as was expected, the incidence of OSA in patients with schizophrenia was higher in the long stay population than in the general population. As we found the Stop bang scale score to be three times higher in-patient score (one) than patients score (three). The screening with the Stop-Bang method, in the majority of the study population, did show a high risk of sleep apnoea in 69% of the whole study group. The same thing was observed in one study done by [27] for psychiatric patients with a high risk of OSA as it was noticed that 62% had a diagnosis of schizophrenia, while the highest risk of apnoea was found in patients treated with Clozapine and Risperidone.
Among our study there were 18 patient scored (one) (a low risk of OSA), 12 scored (two) (an intermediate risk of OSA) and 6 scored (three) (a high risk of OSA). This matches the results of many studies as the one by [28] where he mentioned that high rates of obstructive sleep apnoea symptoms were present in patients with schizophrenia. In addition to [29] who found schizophrenic patients to be at increased risk of OSA compared to non-schizophrenic controls, and his study confirmed the existence of some known risk factors for OSA, including male gender, obesity, hypertension, hyperlipidaemia, diabetes, and antipsychotic use (duration <1 year).
Keeping with literature explaining the pathogenesis of OSA, studies involving schizophrenic participants emphasized on body weight and argued that weight gain among schizophrenic patients due to life style and antipsychotic induced weight gain resulted in OSA [30].
We did not forget while starting this study that obesity is a major risk factor for sleep apnoea, and that in schizophrenia it is twice as frequent as in the general population. That was very true as we found that only 4 patients (11.1%) out of 36 studied has normal body weight , while 7 (19.4%) out of 36 have overweight, and 25 (69.4%) have obesity. There were many obese patients in the sample about 2/3 of the sample were obese. Studies of the same type confirmed our results as that one by Katarzyna [31], where they realised that OSA was more frequent in obese schizophrenia patients than in those consecutively admitted to hospital (45% vs. 22%, (p<0.05). While they found significant differences between patients with and without OSA on the PANSS negative symptoms subscale, B-CATS digit symbol test, and in daytime sleepiness. Our findings match somehow another study done by James [32] in Nigeria, who found that a fifth of in-patients in their exploratory study were at high risk for OSA by using the Berlin questionnaire. And he noticed that patients who are at high risk for OSA were on average overweight, older, using atypical antipsychotics and receiving inpatient care for schizophrenia. In addition to this there is one other study by Annamalai et al. that supports the overweight theory where BMI was significantly higher in a group with an OSA diagnosis compared to those who did not report a diagnosis or treatment for OSA. But what was really new is that they noticed among patients who did not have a diagnosis of OSA but only had a high risk, a non-significant difference in the mean BMI compared with those who were at low risk. Explain which can be possible that patients with a higher BMI have more severe OSA symptoms increasing the likelihood of referral for diagnostic sleep studies.
The long stay words in KCMH carries a variety of factors which can account for the overweight observation which can include one is the general health decline and reduced ability of schizophrenia patients to engage in behaviors such as exercising as they lead a more sedentary way of life than schizophrenic patients in the outside. The second thing is that patients do not maintain a healthful diet where they are able to order junk food if they refuse hospital food [33]. Did prove in there study in 2018 that weight per se is significantly associated with both atypical antipsychotic medications and obstructive sleep apnoea.
Again, there is evidence, however inconsistent, that smoking and drinking alcohol increases the risk of OSA. Both of these behaviors are very common in people with schizophrenia, and sure in our sample that could potentially increase the risk of OSA even more [34].
Regarding waist size we found that more than 38 cm measurements was in 29 patients (80%), indicating an increase in developing truncal obesity and a direct positive relation to OSA. This was proved in one study done by [35] of the interrelation between medications, waist circumference, FVC (percentage), time spent with SaO2<90% during sleep, and the presence of OSA. Where researchers realised that the typical patient with OSA was a man, suffering from schizophrenia and complaining about sleepiness with central obesity, as expressed by (waist circumference), and disturbed daytime respiratory function, as expressed by (FVC).
Previous studies have shown poor rates of measurement of waist circumference by providers in mental health treatment settings even though it is recommended for antipsychotic drug monitoring. It is even less likely that providers will consistently measure neck circumference [36].
Conclusion
This study showed the importance of sleep apnoea diagnosis within mental ill populations that may cause more distress and handicap. There is a high prevalence of OSA symptoms among patients with schizophrenia in long stay rehab wards.
Only a number of patients are screened for OSA when they show symptoms for apnoea. There are clear association between OSA and mental illness. OSA can be identified by using standardized screening tools.
OSA increases cardiovascular risk, affects quality of life, and is associated with cognitive deficits. Early identifications lead to early intervention that can lead to reduce rate of mortality among long stay patient with mental illness in psychiatric wards.
Stop bang is a brief, easy to use standard screening tool for OSA in individuals with mental disorders. Medical and nonmedical professionals can use it. A positive result need to be confirmed by golden standard test such as polysomnography.
If we consider the above discussion, our primary prevention by targeting obesity and lowering BMI may be the most effective (and cost effective) strategy to reduce the comorbidity associated with OSA among individuals with severe mental illness.
A further research is needed to explore those issues among psychiatric patients during their admission.
References
- Adriana F, Albert B, Joaquim R, et al.Cortical gray matter reduction precedes transition to psychosis in individuals at clinical high-risk for psychosis: A voxel-based meta-analysis. Res 232, 98-106 (2021). [Crossref][GoogleScholar][Indexed]
- Werner FM, Rafael C. Risk genes in schizophrenia and their importance in choosing the appropriate antipsychotic treatment. Pharm. Des (2021). [Crossref][Google Scholar][Indexed]
- Bodizs R, Lazar AS. Schizophrenia, slow wave sleep and visuospatial memory: sleep-dependent consolidation or trait-like correlation? Psychiatr. Res 40(1), 89-90 (2006). [Crossref][Google Scholar]
- Göder R, Aldenhoff JB, Boigs M, et al. Delta power in sleep in relation to neuropsychological performance in healthy subjects and schizophrenia patients. Neuropsychiatry. Clin. Neurosci 18(4), 529-535 (2006). [Crossref][Google Scholar][Indexed]
- Daniel Freeman, Bryony Sheaves, Felicity Waite, et al.Oxon Sleep disturbance and psychiatric disorders. Psychiatry 7(7), 628-637 (2020). [Crossref][Google Scholar][Indexed]
- Rachel EK, Bianca G, Fabio F. Schizophrenia and sleep disorders: links, risks, and management challenges. Sci. Sleep 9, 227-239 (2017). [Crossref][Google Scholar][Indexed]
- Afonso P, Figueira ML, Paiva T. Sleep-wake patterns in schizophrenia patients compared to healthy controls. J. Biol. Psychiatry 15(7), 517-524 (2014). [Crossref][Google Scholar][Indexed]
- Melanie ML, Nitin YB, Allan IP, et al. Global burden of sleep-disordered breathing and its implications. Respirology 25(7), 690-702 (2020). [Crossref][Google Scholar][Indexed]
- Stubbs B, Vancampfort D, Veronese N, et al.The prevalence and predictors of obstructive sleep apnea in major depressive disorder, bipolar disorder and schizophrenia: a systematic review and meta-analysis. Affect. Disord 197, 259-267 (2016). [Crossref][Google Scholar][Indexed]
- Sharma P, Dikshit R, Shah N, et al.Excessive daytime sleepiness in schizophrenia: a naturalistic clinical study. Clin. Diagn. Res 10(10), VC06-VC08 (2016). [Crossref] [Google Scholar][Indexed]
- Alam A, Chengappa KR, Ghinassi F. Screening for obstructive sleep apnea among individuals with severe mental illness at a primary care clinic. Hosp. Psychiatry 34(6), 660-664 (2012). [Crossref][Google Scholar][Indexed]
- Kaskie RE, Graziano B, Ferrarelli. Schizophrenia and sleep disorders: links, risks, and management challenges. Sci. Sleep 9, 227-239 (2017). [Crossref][Google Scholar][Indexed]
- Anderson, Curtin, Higgins, et al. Screening for obstructive sleep apnea in inpatients
with schizophrenia: A feasibility study. N. Z. J. Psychiatry 52(9), 898-899 (2018). [Crossref][Google Scholar][Indexed] - Aniyizhai A, Cenk T. An overview of diabetes management in schizophrenia patients: office based strategies for primary care practitioners and endocrinologists. J. Endocrinol 2015, 969182 (2015). [Crossref][Google Scholar][Indexed]
- Ancoli IS, Martin J, Jones DW, et al.Sleep-disordered breathing and periodic limb movements in sleep in older patients with schizophrenia. Psychiatry 5(11), 1426-1432 (1999). [Crossref][Google Scholar][Indexed]
- Zanini MA, Castro J, Cunha GR, et al.Abnormalities in sleep patterns in individuals at risk for psychosis and bipolar disorder. Res 169(1), 262-267 (2015). [Crossref][Google Scholar][Indexed]
- Cohrs, S. Sleep Disturbances in Patients with Schizophrenia Impact and Effect of Antipsychotics. Drugs 22(11), 939-962 (2008). [Crossref][Google Scholar][Indexed]
- Lunsford AJR, Le Bourgeois MK, Gupta T, et al.Actigraphic-measured sleep disturbance predicts increased positive symptoms in adolescents at ultra high-risk for psychosis: a longitudinal study. Res 164(1), 15-20 (2015). [Crossref][Google Scholar][Indexed]
- Castelnovo A, D'Agostino A, Casetta C, et al.Sleep spindle deficit in schizophrenia: contextualization of recent findings. Psychiatry. Rep 18(8), 1-10 (2016). [Crossref][Google Scholar][Indexed]
- Afonso P, Brissos S, Figueira ML, et al.Schizophrenia patients with predominantly positive symptoms have more disturbed sleep-wake cycles measured by actigraphy. Res 189(1), 62-66 (2011). [Crossref][Google Scholar][Indexed]
- Afonso P, Brissos S, Cañas F, et al.Treatment adherence and quality of sleep in schizophrenia outpatients. J. Psychiatry. Clin. Pract 18(1), 70-76 (2014). [Crossref][Google Scholar][Indexed]
- Mulligan LD, Haddock G, Emsley R, et al.High resolution examination of the role of sleep disturbance in predicting functioning and psychotic symptoms in schizophrenia: a novel experience sampling study. Abnorm. Psychol 125(6), 788-797 (2016). [Crossref][Google Scholar][Indexed]
- Jannis N, Nikos AV, Styliani S, et al. Assessment of visuo-spatial memory in patients with schizophrenia using the location learning test. AUMJ 37(1), 199459110 (2010). [CrossRef][Google Scholar]
- Waite F, Evans N, Myers E, et al.The patient experience of sleep problems and their treatment in the context of current delusions and hallucinations. Psychother 89(2), 181-193 (2016). [Crossref][Google Scholar][Indexed]
- Chamara VS, Jennifer LP, Caroline JL, et al. Prevalence of obstructive sleep apnea in the general population: A systematic review. Med. Rev 34, 70-81 (2017). [Crossref][Google Scholar][Indexed]
- Lin WC, Winkelman JW. Obstructive sleep apnea and severe mental illness: evolution and consequences. Psychiatry. Rep 14(5), 503-510 (2012). [Crossref][Google Scholar][Indexed]
- Rupali R, Ravi G, Rajat R, et al.Is obstructive sleep apnea the missing link between metabolic syndrome and second-generation antipsychotics: Preliminary study. J. Psychiatry 60(4), 478-484 (2018). [Crossref][Google Scholar][Indexed]
- Annamalai A, Palmese LB, Chwastiak LA, et al.High rates of obstructive sleep apnea symptoms among patients with schizophrenia.Psychosomatics 56, 59-66 (2015). [Crossref][Google Scholar][Indexed]
- Ying Ying Wu, En Ting Chang, Yu Cih Yang, et al.Risk of obstructive sleep apnea in patients with schizophrenia: a nationwide population-based cohort study. Psychiatry. Psychiatr. Epidemiol 55(12), 1671-1677 (2020). [Crossref][Google Scholar][Indexed]
- Xu S, Wan Y, Xu M, et al.The association between obstructive sleep apnea and metabolic syndrome: A systematic review and meta-analysis. Pulm. Med 15, 105 (2015). [Crossref][Google Scholar][Indexed]
- Katarzyna S, Adam W. Simple assessment of risk of obstructive sleep apnea in schizophrenia. Psychiatr. Res 125, 33-37 (2020). [Crossref][Google Scholar][Indexed]
- James BO, Inogbo CF, Archibong AO. Risk of obstructive sleep apnoea syndrome among in-patients at a neuropsychiatric hospital in Nigeria: A short report. Health. Sci 15(3), 967-971 (2015). [Crossref][Google Scholar][Indexed]
- Khazaie H, Sharafkhaneh A, Khazaie S, et al.A weight-independent association between atypical antipsychotic medications and obstructive sleep apnea. Breath 22(1), 109-114 (2018). [Crossref][Google Scholar][Indexed]
- Beat K, Nicholas TE, Pantelis T, et al.Clinical characteristics of obstructive sleep apnea in psychiatric disease. Clin. Med 8(4), 534 (2019). [Crossref][Google Scholar][Indexed]
- Barber J, Palmese L, Chwastiak LA, et al.Reliability and practicality of measuring waist circumference to monitor cardiovascular risk among community mental health center patients. Ment. Health. J 50(1), 68-74 (2014). [Crossref][Google Scholar][Indexed]
- Rishi MA, Shetty M, Wolff A, et al.Atypical antipsychotic medications are independently associated with severe obstructive sleep apnea. Neuropharmacol 33(3), 109-113 (2010). [Crossref][Google Scholar][Indexed]