Research Article - (2018) Volume 8, Issue 6
Comparison of the Defined Daily Dose and Chlorpromazine Equivalent Methods in Antipsychotic Drug Utilization in Six Asian Countries
- Corresponding Author:
- Shih-Ku Lin, MD
Taipei City Hospital and Psychiatric Center, 309 Songde Road, Taipei 110, Taiwan
Tel: 886227263141
Abstract
Background:
The defined daily dose (DDD) from the Anatomical Therapeutic Chemical Classification System can be utilised as a reference for international drug utilization research, according to the World Health Organization. Alternatively, chlorpromazine equivalent (CPZeq) is a traditional method that has been used to indicate the dose of antipsychotics for decades. The aim of this study was to investigate and compare the DDD and CPZeq methods in order to calculate the total antipsychotic dose of inpatients with schizophrenia.
Methods and Findings:
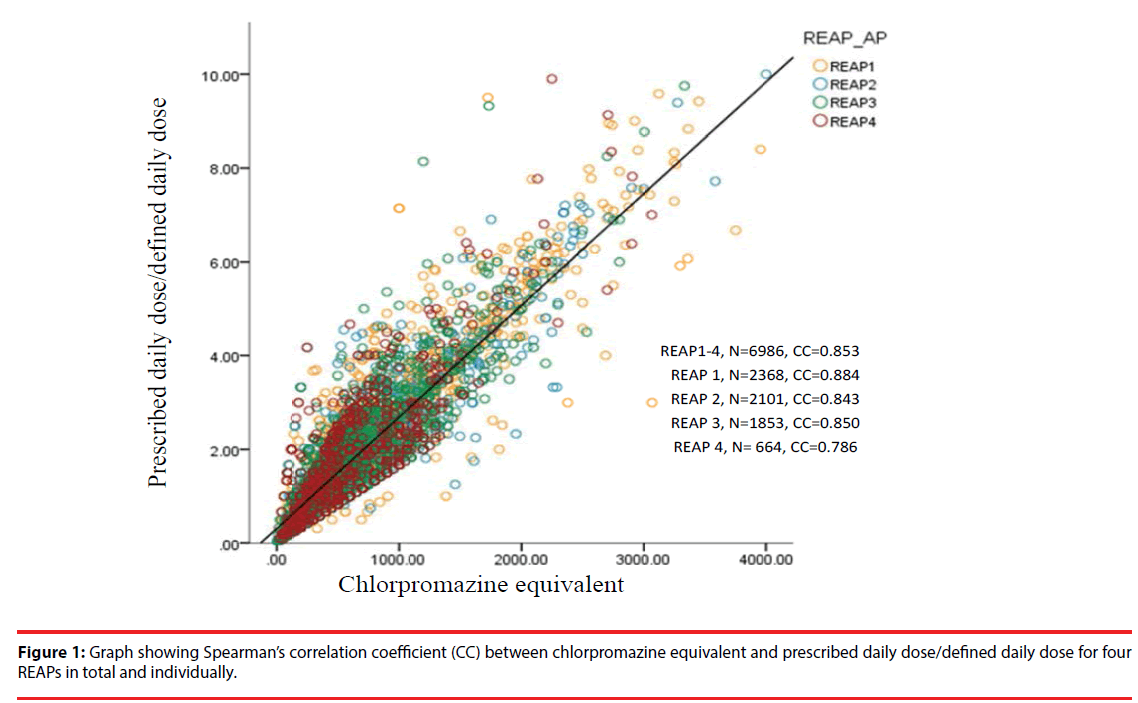
Six countries (China, Hong Kong, Japan, Korea, Singapore, and Taiwan) participated in antipsychotic prescription pattern surveys conducted four times during 2001, 2004, 2009, and 2016. The antipsychotic loading (APL) values of each prescription, calculated using the DDD and CPZeq methods, and their correlations were compared. A total of 6986 prescriptions from inpatients with schizophrenia were analysed. Spearman’s correlation coefficients (CCs) between the DDD and CPZeq were 0.853 overall, and 0.884, 0.843, 0.850, and 0.786 for the individual surveys (1–4, respectively). The CC of FGA only (n=2442), SGA only (n=2992) and combination of FGA and SGA (n=1552) were 0.901, 0.757, and 0.883, respectively. The mean APL values calculated by the DDD and CPZeq methods were 1.73 ± 1.40 and 597.0 ± 530.7 mg, respectively.
Conclusions:
Significant correlations between the DDD and CPZeq methods were observed. The decreasing trend in CC values from the first to the fourth survey might be attributed to the more common use of second-generation antipsychotics in recent years. We suggest that DDD method is more applicable in clinical practice and drug utilization research since other psychotropic drug such as mood stabilizers or anxiolytics can be calculated together.
Keywords
Defined daily dose, Chlorpromazine equivalent, Antipsychotic, Drug loading
Introduction
Antipsychotics are a class of psychotropic medications used to manage psychotic symptoms. In general, the main indication of antipsychotic drugs is schizophrenia. Clinically, information about the potency of a specific antipsychotic is necessary prior to initial prescription, switching from one antipsychotic to another, or combing two or more drugs simultaneously. Chlorpromazine (CPZ) was the first antipsychotic, and the CPZ equivalent (CPZeq) is a measure of the relative antipsychotic potencies. In 1974, Davis was the first to propose the dose equivalence of antipsychotic drugs using the CPZeq concept [1]. He surveyed 56 double-blind clinical trials using CPZ as a standard, directly or indirectly, and suggested a dose ratio equivalent to 100 mg of CPZ for each antipsychotic drug. The CPZeq method has been widely applied for decades to compare the dosage equivalence of most antipsychotics, with some modifications in the original figures of the first-generation antipsychotics (FGAs) [2] and depot antipsychotics suggested by Kane et al. [3]. For second-generation antipsychotics (SGAs), Woods [4] proposed a figure based on available fixed-dose placebo-controlled studies. However, dose equivalents for the newer antipsychotics such as iloperidone, lurasidone, and paliperidone are not available [5].
In 2003, the World Health Organization (WHO) developed the Anatomical Therapeutic Chemical (ATC) classification and the defined daily dose (DDD) system for international drug utilization studies. The DDD is the assumed average maintenance dose of a drug per day for its main indication in adults of 70 kg [6]. The DDD system incorporates all drugs available on the market including antipsychotics (https://www.whocc.no/atc_ddd_index/ [accessed 15 September 2016]).
Nose et al. [7] analysed the relationship between the daily doses of antipsychotics (expressed as DDDs), CPZeq, and percentages of the British National Formulary (BNF) maximum recommended daily dose in 277 patients with schizophrenia. The results revealed significant correlations between DDDs and CPZeq (Spearman’s r = 0.779, P < 0.001) and between DDDs and the percentages of the BNF maximum recommended daily dose (Spearman’s r = 0.869, P < 0.001), thus indicating the reliability of the DDD system as a tool for standardising antipsychotic doses in studies involving drug utilisation. In this study, the type such as FGA or SGA was not mentioned and the patient number was small. As newer antipsychotics are getting popularly used in recent decade, it is warranted to clarify the correlation of DDD and CPZ methods in a large sample and different time frame.
The Research on Asian Prescription Patterns (REAP) is an international collaborative consortium for studying prescription patterns of psychotropic drugs across countries in this region. It had conducted four surveys on antipsychotics (REAP-1, -2, -3 and -4 in 2001, 2004, 2009 and 2016, respectively; http://reap.asia/index.html). The aim of the present study was to further investigate and compare the DDD and CPZeq methods for the calculation of total antipsychotic doses among inpatients with schizophrenia from the REAP-1 to REAP-4 database.
Methods
Six countries, namely China, Hong Kong, Japan, South Korea, Singapore, and Taiwan, had consecutively participated in four surveys on the use of psychotropic drugs in inpatients with schizophrenia; the details of the REAP study have been described previously [8,9], and are summarised in the following paragraph.
Briefly, participating patients met the following study criteria: (i) International Statistical Classification of Diseases and Related Health Problems (ICD)-10 or Diagnostic and Statistical Manual of Mental Disorders (DSM)- IV diagnosis of schizophrenia; (ii) ability to comprehend the aims of the study; and (iii) willingness to provide written or oral consent according to the requirements of the clinical research ethics committees in the respective study sites. Consensus meetings on data collection and uniformity of data entry were held before each survey. Sociodemographic and clinical characteristics including age, sex, and type and doses of all psychotropic drugs prescribed, including antipsychotics, mood stabilisers, antidepressants, anxiolytics, and hypnotics, were collected by the attending psychiatrists of the patients or by members of the research team with the agreement of the psychiatrist in charge of the patient.
The daily doses of antipsychotic drugs in each prescription were converted into antipsychotic loading (APL) using the DDD (prescribed daily dose/DDD) and CPZeq methods [2-4]. For patients prescribed more than one antipsychotic drug, the APL was calculated by summing the prescribed daily dose/DDD or CPZeq of each antipsychotic.
▪ Statistical analyses
We used SPSS for Windows (version 20; IBM Corp., Armonk, NY, USA) to compute the study data. Correlations between the APL expressions obtained using the DDD and CPZeq methods were investigated using the Spearman’s rank correlation coefficient (CC). Multivariable linear regression was used to compare the CCs between groups. Statistical significance was set at P < 0.05.
Results
A total of 6986 prescription forms from inpatients with schizophrenia (mean age, 44.2 ± 13.8 years) were analysed. Table 1 shows the number of patients from the six countries. The mean APL obtained using DDD was 1.73 ± 1.40, whereas that obtained using CPZeq was 597.0 ± 530.7 mg. Figure 1 compares the Spearman’s CCs of the correlations between the CPZeq and DDD methods for all four REAPs and for individual surveys from REAP-1 to REAP-4, all of which demonstrated statistical significance (P < 0.001). Multivariable linear regression revealed that the CC for REAP-4 was significantly lower than those of the previous three surveys (P < 0.001). Table 2 compares the frequencies (number and percent) of the 30 most used antipsychotics (individual and total). Since polypharmacy use was popular in this data set (43.2% in total), it accounted for 155.2% (in total) of the 30 most used antipsychotics in this study. Trends in the decreased use of FGAs only (53.0% in REAP-1 to 8.9% in REAP-4) and increased use of SGAs only (27.3% in REAP-1 to 62.5% in REAP-4) were noted. The most used antipsychotic in total was risperidone (27.3%), whereas that among the individual REAPs was olanzapine (30.3% in REAP-4). The CC of FGAs only (n = 2442), SGAs only (n = 2992), and the combination of FGAs and SGAs (n = 1552) were 0.901, 0.757, and 0.883, respectively. The CC of SGAs only was significantly lower than that of FGAs only in the multivariable linear regression analysis (P < 0.001).
| China | Hong Kong | Singapore | Taiwan | Korea | Japan | Total | |
|---|---|---|---|---|---|---|---|
| Male | 937 | 163 | 318 | 887 | 653 | 1053 | 4011 |
| Female | 699 | 144 | 293 | 586 | 473 | 780 | 2975 |
| Total | 1636 | 307 | 611 | 1473 | 1126 | 1833 | 6986 |
Table 1: Number of patients in six countries.
| Antipsychotic Class | REAP-1 | REAP-2 | REAP-3 | REAP-4 | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | ||
| Risperidone | Sga | 472 | 19.9 | 640 | 30.5 | 607 | 32.7 | 189 | 28.5 | 1908 | 27.3 |
| Haloperidol | Fga | 724 | 30.6 | 413 | 19.7 | 364 | 19.6 | 56 | 8.4 | 1557 | 22.3 |
| Chlorpromazine | Fga | 561 | 23.7 | 349 | 16.6 | 184 | 9.9 | 47 | 7.1 | 1141 | 16.3 |
| Clozapine | Sga | 348 | 14.7 | 340 | 16.2 | 297 | 16 | 141 | 21.2 | 1126 | 16.1 |
| Olanzapine | Sga | 114 | 4.8 | 226 | 10.8 | 289 | 15.6 | 201 | 30.3 | 830 | 11.9 |
| Sulpiride | Fga | 232 | 9.8 | 178 | 8.5 | 114 | 6.2 | 39 | 5.9 | 563 | 8.1 |
| Levomepromazine | fga | 246 | 10.4 | 165 | 7.9 | 139 | 7.5 | 12 | 1.8 | 562 | 8 |
| Quetiapine | sga | 86 | 3.6 | 167 | 8 | 214 | 11.5 | 88 | 13.3 | 555 | 7.9 |
| Zotepine | sga | 137 | 5.8 | 107 | 5.1 | 108 | 5.8 | 34 | 5.1 | 386 | 5.5 |
| Flupentixol | fga | 112 | 4.7 | 66 | 3.1 | 55 | 3 | 55 | 8.3 | 288 | 4.1 |
| Fluphenazine | fga | 149 | 6.3 | 49 | 2.3 | 49 | 2.6 | 1 | 0.2 | 248 | 3.6 |
| Trifluoperazine | fga | 114 | 4.8 | 41 | 2 | 44 | 2.4 | 6 | 0.9 | 205 | 2.9 |
| Zuclopenthixol | fga | 72 | 3 | 38 | 1.8 | 40 | 2.2 | 26 | 3.9 | 176 | 2.5 |
| Bromperidol | fga | 79 | 3.3 | 53 | 2.5 | 15 | 0.8 | 4 | 0.6 | 151 | 2.2 |
| Aripiprazole | sga | 0 | 0 | 0 | 0 | 106 | 5.7 | 40 | 6 | 146 | 2.1 |
| Perphenazine | fga | 62 | 2.6 | 45 | 2.1 | 27 | 1.5 | 6 | 0.9 | 140 | 2 |
| Thioridazine | fga | 67 | 2.8 | 40 | 1.9 | 2 | 0.1 | 0 | 0 | 109 | 1.6 |
| Amisulpride | sga | 0 | 0 | 22 | 1.1 | 47 | 2.5 | 37 | 5.6 | 106 | 1.5 |
| Nemonapride | fga | 44 | 1.9 | 46 | 2.2 | 9 | 0.5 | 0 | 0 | 99 | 1.4 |
| Perospirone | sga | 15 | 0.6 | 40 | 1.9 | 34 | 1.8 | 3 | 0.5 | 92 | 1.3 |
| Propericiazine | fga | 43 | 1.8 | 23 | 1.1 | 17 | 0.9 | 2 | 0.3 | 85 | 1.2 |
| Sultopride | fga | 40 | 1.7 | 24 | 1.1 | 17 | 0.9 | 2 | 0.3 | 83 | 1.2 |
| Pipotiazine | fga | 42 | 1.8 | 26 | 1.2 | 13 | 0.7 | 1 | 0.2 | 82 | 1.2 |
| Paliperidone | sga | 0 | 0 | 0 | 0 | 17 | 0.9 | 34 | 5.1 | 51 | 0.7 |
| Ziprasidone | sga | 0 | 0 | 10 | 0.5 | 24 | 1.3 | 6 | 0.9 | 40 | 0.6 |
| Clotiapine | fga | 11 | 0.5 | 7 | 0.3 | 8 | 0.4 | 12 | 1.8 | 38 | 0.5 |
| Blonanserin | fga | 0 | 0 | 0 | 0 | 24 | 1.3 | 12 | 1.8 | 36 | 0.5 |
| Mosapramine | fga | 10 | 0.4 | 3 | 0.1 | 0 | 0 | 2 | 0.3 | 15 | 0.2 |
| Pipameperone | fga | 9 | 0.4 | 3 | 0.1 | 0 | 0 | 1 | 0.2 | 13 | 0.2 |
| Penfluridol | sga | 4 | 0.2 | 3 | 0.1 | 0 | 0 | 1 | 0.2 | 8 | 0.1 |
| Total | 3793 | 160.2 | 3124 | 148.8 | 2864 | 154.5 | 1058 | 159.3 | 10839 | 155.2 | |
Table 2: Comparison of the number (N) and percentage (%) of specific antipsychotics in each survey.
The suggested DDD of CPZ is 300 mg by WHO; hence, the antipsychotic loading represented by CPZeq/300 mg was compared with prescribed daily dose/DDD among the countries in the four surveys (Table 3). Japan presented with the highest antipsychotic quantity (2.51/2.26) and China with the lowest (1.62/1.31). In total, the antipsychotic loading, as represented by CPZeq, was approximately 15% higher than that of the DDD method.
| China | Hong Kong | Singapore | Taiwan | Korea | Japan | Average | Ratio | |
|---|---|---|---|---|---|---|---|---|
| REAP-1 | 1.48/1.16 | 1.85/1.61 | 2.01/2.01 | 1.63/1.44 | 2.29/1.94 | 3.03/2.46 | 2.14/1.81 | 1.18 |
| REAP-2 | 1.54/1.13 | 1.63/1.35 | 1.78/1.60 | 1.65/1.39 | 2.18/1.84 | 2.26/2.06 | 1.89/1.60 | 1.18 |
| REAP-3 | 1.81/1.55 | 1.66/1.48 | 1.32/1.34 | 1.65/1.37 | 2.42/2.05 | 2.12/2.13 | 1.92/1.73 | 1.11 |
| REAP-4 | 1.95/1.88 | 1.61/1.69 | 1.69/1.64 | 1.72/1.60 | 4.31/3.57 | 2.71/2.71 | 1.98/1.89 | 1.05 |
| Total | 1.62/1.31 | 1.71/1.48 | 1.80/1.76 | 1.65/1.43 | 2.29/1.94 | 2.51/2.26 | 1.99/1.73 | 1.15 |
Table 3: Antipsychotic loading calculated using the CPZeq/300 mg and PDD/DDD methods for the six countries during the four REAP surveys.
Discussion
The principal finding of this large-scale study is the confirmation of the fact that both the DDD and CPZeq methods are compatible tools for the standardisation of antipsychotic doses in drug-utilisation research (CC = 0.853). A study comparing the correlation between DDD and CPZeq in 250 patients with schizophrenia reported a Spearman’s CC of 0.92 [10]; the study revealed that the coherence was strongest when dealing with FGAs. The results from our study also showed that the CCs for the correlations between the CPZeq and DDD methods were significantly lower in SGAs than in FGAs. Moreover, the decrease in the Spearman’s CC from REAP-1, -2, and -3 to REAP-4 might be attributed to the more common use of SGAs in recent years (Table 2). The current largescale survey of inpatients demonstrated that the mean daily doses represented by APL were 99% and 73% higher using the CPZeq and DDD methods, respectively, than the maintenance dose suggested by DDD/ATC system (Table 3). Thus, this suggested that inpatients with schizophrenia require almost double doses in the acute phase compared with maintenance phase. These findings may help clinicians during antipsychotic dose judgment and health authorities during policymaking. Notably, the current study revealed variation in APL among the countries, where Korea and Japan used higher, and China and Taiwan used lower antipsychotic dosage.
The concept of CPZeq was derived from the potency for dopamine receptor blockade, which was determined empirically to judge the dose equivalence between different antipsychotic agents [1]. Because most of the SGAs were serotonin-dopamine antagonists, it was difficult to predict such an equivalence, leading to the introduction of the minimum effective dose method by Woods [4]. The author identified the minimum effective dose of several newer atypical antipsychotic drugs based on fixed-dose placebo-controlled studies, and then obtained the individual CPZeq. Using the same method, Leucht et al. [11] analysed 73 clinical trials and recommended another set of minimal effective doses for specific antipsychotics. This concept is highly similar to the DDD system, in which the maintenance dose of a drug per day is suggested for its main indication in adults weighing 70 kg. However, in another study, the same group recommended the use of alternative, more ‘scientific’ dose equivalence methods for a drug, if available [12], because the information used to estimate DDDs is likely to differ between drugs and is not publicly available. In an early study comparing the CPZeq and DDD systems in 33 antipsychotics including atypical ones such as clozapine, risperidone, quetiapine, olanzapine, ziprasidone, and sertindole, a major discrepancy between the two methods was observed because nearly 67% of the DDD-equivalent values demonstrated lower potencies when compared with the CPZ-equivalent values for each drug [13]. The authors suggested that DDDs might present a more reliable method for comparing both typical and atypical antipsychotic doses than CPZeq. Notably, in the present study, the APL in total prescriptions was approximately 15% (1.99/1.73; Table 3) higher with the CPZeq method than with the DDD method, meaning that DDD-equivalent revealed lower potencies too. Inada and Inagaki [14] determined the dose equivalents of antipsychotics based on randomised controlled trials conducted in Japan and consensus among dose equivalency reported previously by psychopharmacological experts. In general, their suggested daily doses were slightly lower than that of the Western reports. Table 4 compares the various aforementioned methods, wherein the CPZ was set as 300 mg per day as a maintenance dose.
| DDD/ATC | CPZeq x3[2]* | Woods [4] | Leucht [11] | Inada [14] | |
|---|---|---|---|---|---|
| Amisulpride | 400 | 300 | − | − | − |
| Aripiprazole | 15 | 22.5 | 15 | 10 | 12 |
| Asenapine | 20 | 15 | − | 10 | − |
| Clozapine | 300 | 150 | − | 300? | 150 |
| Chlorpromazine | 300 | 300 | 200 | 250 | 300 |
| Haloperidol | 8 | 6 | 4 | 4 (4.5) | 6 |
| Iloperidone | 18 | 18 | − | 8 (12) | − |
| Lurasidone | 60 | 60 | − | 40 | − |
| Olanzapine | 10 | 15 | 10 | 7.5 (10) | 7.5 |
| Paliperidone | 6 | 4.5 | − | 3 (6) | 4.5 |
| Quetiapine | 400 | 225 | 150 | 150 (250) | 200 |
| Risperidone | 5 | 6 | 4 | 2 (4) | 3 |
| Sertindole | 16 | − | − | 12 (16) | − |
| Ziprasidone | 80 | 180 | 120 | 40 (80) | − |
| Zotepine | 200 | 200 | − | − | 200 |
Table 4: Comparison of different daily dose equivalent methods.
The combination of medications with antipsychotics such as mood stabilizers, antidepressants, and anxiolytics is a prominent treatment strategy for schizophrenia and bipolar disorder. Since CPZeq is only for antipsychotics, while the DDD system consist of most of the marketed medications including psychotropic drugs, making it easier to apply, particularly when comparing the dosages of concomitant medications other than antipsychotics.
Acknowledgements
The authors thank Mr Da-Yi Tsai for internet server maintenance and Mr Yan-Lung Chiou for assistance with data management. This manuscript was edited by Wallace Academic Editing.
Authors’ Contribution
NS, MC, and CT designed the REAP survey and all authors participated in this study. SL and SY were responsible for data collection and analysis. SL wrote the first draft of the manuscript, and all other authors reviewed the results and contributed to the final draft of the manuscript.
Declaration
All authors declare that they have no conflict of interest in reporting this study.
Funding
This work was supported by Taipei City Government (10501-62-012) and Ministry of Science and Technology, Taiwan (106-2314-B-532 -009).
References
- Davis JM. Dose equivalence of the antipsychotic drugs. J. Psychiatr. Res 11, 65-69(1974).
- APA. Practice Guideline for the Treatment of Patients with Schizophrenia Washington, DC: American Psychiatric Press (1997).
- Kane JM, Aguglia E, Altamura AC et al. Guidelines for depot antipsychotic treatment in schizophrenia. European Neuropsychopharmacology Consensus Conference in Siena, Italy. Eur. Neuropsychopharmacol 8(1), 55-66 (1998).
- Woods SW. Chlorpromazine equivalent doses for the newer atypical antipsychotics. J. Clin. Psychiatry 64(6), 663-7 (2003).
- Leucht S, Samara M, Heres S et al. Dose Equivalents for Second-Generation Antipsychotic Drugs: The Classical Mean Dose Method. Schizophr. Bull 41(6), 1397-1402 (2015).
- WHO Collaborating Centre for Drug Statistics and Methodology [http://www.who.int/medicines/regulation/medicines-safety/about/collab-centres-norwegian/en/]
- Nose M, Tansella M, Thornicroft G et al. Is the Defined Daily Dose system a reliable tool for standardizing antipsychotic dosages? Int. Clin. Psychopharmacol 23(5), 287-290 (2008).
- Chong MY, Tan CH, Fujii S et al. Antipsychotic drug prescription for schizophrenia in East Asia: rationale for change. Psychiatry Clin, Neurosci 58(1), 61-67 (2004).
- Xiang YT, Wang CY, Si TM et al. Antipsychotic polypharmacy in inpatients with schizophrenia in Asia (2001-2009). Pharmacopsychiatry 45(1), 7-12(2012).
- Sweileh WM, Odeh JB, Shraim NY et al. Evaluation of Defined Daily Dose, percentage of British National Formulary maximum and chlorpromazine equivalents in antipsychotic drug utilization. Saudi. Pharm. J 22(2), 127-132 (2014).
- Leucht S, Samara M, Heres S et al. Dose equivalents for second-generation antipsychotics: the minimum effective dose method. Schizophr. Bull 40(2), 314-326 (2014).
- Leucht S, Samara M, Heres S, Davis JM. Dose Equivalents for Antipsychotic Drugs: The DDD Method. Schizophr. Bull 42 Suppl 1, S90-94 (2016).
- Rijcken CA, Monster TB, Brouwers JR, de Jong-van den Berg LT. Chlorpromazine equivalents versus defined daily doses: how to compare antipsychotic drug doses? J. Clin. Psychopharmacol 23(6), 657-659 (2003).
- Inada T, Inagaki A. Psychotropic dose equivalence in Japan. Psychiatry Clin Neurosci 69(8), 440-447 (2015).