Research Article - Neuropsychiatry (2017) Volume 7, Issue 5
Acupuncture for Non-Verbal Autistic Children: A Small Case Series
- Corresponding Author:
- Dr. Wen-Xiong Chen (M.D. Ph.D.)
Department of Neurology, Brain Center, Guangzhou Women and Children’s Medical Center
Guangzhou Medical University, 9# Jin Sui Road, 510623, Guangzhou City, Guangdong Province, P.R. of China
Tel: 86-020-38076127
Abstract
Background:
Severe speech deficit is difficult to treat autistic characteristics. The dysfunction mirror neuron system is thought to be related to autism communication, social and emotion regulation. Hypothetically acupuncture may serve as an ideal intervention method to adjust the dysfunction MNS, via its corresponding acupoints.
Objective:
To observe for efficacy and safety of acupuncture for non-verbal autistic children.
Methods:
Five non-verbal autistic children received acupuncture for 20 sessions over 4 weeks. Assessment tools were adopted pre- and post-acupuncture including Autism Treatment Evaluation Checklist (ATEC) for symptomatology, Gesell Development Diagnosis Scale (GDDS) for developmental quotient (DQ), Reynell Developmental Language Scale (RDLS) for language, Pediatric Evaluation Disability Inventory (PEDI) and Clinical Global Impression-Improvement (CGI-I) scale for functional status.
Results:
For ATEC, non-significant improvement in the “Sociability” domain (p=0.05) was noted, while significant improvement of general DQ (P=0.018) was revealed regarding GDDS, which was attributed to the improvements of sub-domain of fine motor as well as adaptability. For RDLS, there were no significant changes in the comprehension or production domains, while nonsignificant improvement (P=0.052) in the self-care domain of PEDI was revealed. For CGI-I, much improvement was reported in 2 cases, on the “social relatedness and imitation” and “social relatedness and communication” domains respectively, while minimal improvement in other 2 cases and no change in remaining 1 case were also stated. All children were compliant with all acupuncture sessions.
Conclusion:
A short intensive course of acupuncture might improve some core features of non-verbal autistic children. Further high quality trials are needed.
Keywords
Autism Spectrum Disorder (ASD), Acupuncture, Non-verbal, Children, Mirror Neuron System (MNS)
Introduction
Autism spectrum disorder (ASD) is a neurodevelopmental disorder, characterized by the deficits in social relatedness, verbal and non-verbal communication, and stereotypic behaviors [1]. Its heterogeneity has long been concerned, especially in the early language development, ranging from the complete absence of functional speech, to the existence of adequate linguistic knowledge with the impairment in the functional use of that knowledge [2]. Around 25% of individuals with ASD remained without functional speech [3]. Language proficiency is one of most important predicting variables regarding the outcomes of autism [4]. Autism interventions have focused much attention on helping children with autism acquire language [5].
The dysfunction of mirror neuron system (MNS) and its related networks are thought to be related to autism communication, social and emotional regulation [6]. The area of the inferior frontal region, strongly associated with human language, namely Broca area [7], contains MNS [8]. Other areas, such as the top of the inferior parietal and superior temporal sulcus, are also thought to comprise MNS [9]. The MNS is involved in the perception and understanding of human activities, as well as takes part in a higher level of cognitive processing such as imitation and language [10].
The design of an intervention method to the engagement with the MNS mechanism may have an important clinical application potential [11]. Studies have revealed that use of Complementary and Alternative Medicine (CAM) in the pediatric population for treating chronic conditions is estimated to be from 2% to more than 70% [12]. Some CAM therapies such as acupuncture for ASD are reported with promising results, although there is no conclusive evidence supporting the efficacy of CAM therapies in ASD [13]. Acupuncture involves using needles or pressure on specific areas of the body and is an important therapeutic method in Traditional Chinese Medicine [14]. Hypothetically, acupuncture may serves as an ideal intervention method to engage with the MSN mechanism, via its corresponding acupoints.
To date, there is no study regarding the acupuncture for non-verbal autistic children. As a result, we performed a pilot study to observe the efficacy of acupuncture for non-verbal autistic children, as well as to monitor the safety, although recent overview of systematic reviews [15] found only six reviews reported adverse events and no fatal side effects were reported. Current study served as the basis for our randomized controlled trial.
Methods
The current pilot study was conducted from July 2015 to Match 2016 at Guangzhou Women and Children’s Medical Center, Guangzhou Medical University, with the senior author (WX Chen) as principal investigator, in collaboration with the Department of Rehabilitation, the Third Affiliated Hospitals of Southern Medical University. The research protocol was approved by the Institutional Review Board of the Guangzhou Women and Children’s Medical Center. Written informed consents were obtained from the parents/caregivers.
Participants were recruited from a neuropsychological clinic that specializes in ASD. The comprehensive physical examination and evaluation for children with ASD were performed.
Estimates of spontaneous use of functional speech were obtained through a brief interview with the parent, as well as by clinical observation during the developmental and diagnostic assessments. The severity of autism was assessed using Childhood Autism Rating Scale (CARS) [16].
▪ Inclusion criteria
Children with ASD satisfying the following criteria were included in the study:
Diagnostic and Statistical Manual of Mental Disorders (5th edition) (DSM-5) [1].
Autism Diagnostic Interview–Revised (ADI-R) [17].
Autism Diagnostic Observation Schedule (ADOS) [18].
Non-verbal autistic children: spontaneous use of less than five functional words.
Age between 2 and 14 years.
Have not received acupuncture treatment before.
▪ Exclusion criteria
Exclusion criteria were children with associated neurologic disorders e.g. epilepsy.
▪ Intervention
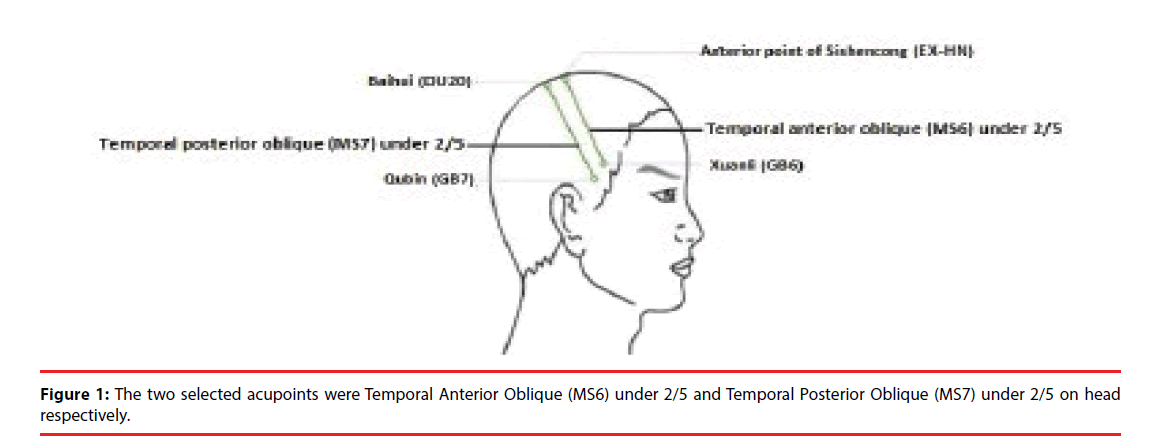
The acupuncture was performed by the acupuncturist (G Liu). The following two acupoints [the temporal anterior oblique (MS6) under 2/5 and temporal posterior oblique (MS7) under 2/5] on head (Figure 1) were selected bilaterally, and were alternately used for acupuncture.
Acupuncture consisted of 20 sessions, with consecutive 5 sessions from Monday to Friday per week, each lasting 30 minutes, spanned over 4 weeks. A sterile disposable 0.3 × 4-cm acupuncture needle (made in SuZhou, China, HWA-TO) was used. During treatment, the patient was required to be in a sitting position. Needle sites were disinfected, and disposable needles were inserted into the acupoints selected.
The children could continue their special education within the special school if he/she had already been accepted it during the acupuncture period. They were advised not to accept other therapies such as alternative medicine during the acupuncture period.
▪ Outcome measures
Parental assessment: The following outcome measures were provided by parents. During the baseline assessment the parents were instructed on how to properly apply the following assessment tools.
Autism Treatment Evaluation Checklist (ATEC) [19]: A scale for rating symptoms of patients with autism before and after intervention, consisting of five subscales Speech/Language/ Communication, Sociability, Sensory/Cognitive Awareness, Health/Physical/Behavior, and Total ATEC Summary Score, used at baseline and post-treatment.
Pediatric Evaluation Disability Inventory (PEDI) [20]: A measure of functional ability in children, taking account the use of special equipment and amount of caregiver assistance, consisting of 197 functional skills items, 20 caregiver assistance activities, and 20 environmental modifications, used at baseline and post-treatment.
Clinical Global Impression-Improvement (CGI-I) Scale [21]: The Clinical Global Impression-Improvement (CGI-I) scale is a seven-point scale that requires the assessor to evaluate how much the subject’s illness has improved or worsened with regard to a baseline state. Subjects were rated on a Likert scale of 1–7, with 1=very much improved, 2 =much improved, 3=minimally improved, 4=no change, 5=minimally worse, 6=much worse, and 7=very much worse, used at post-treatment.
Weekly Parental Report: A self-devised report was used for parents to record weekly changes during acupuncture consisting of opening questions to answer in a written format accordingly.
Assessor assessment: The following outcome measures were performed at baseline and post-treatment by assessor.
Gesell Developmental Diagnostic Scale (GDDS) [22]: A measure developmental quotient (DQ) in the following domains, including gross motor, fine motor, adaptability, language, and personal-social behavior.
Reynell Developmental Language Scale (RDLS) [23]: A measure of a child’s receptive and expressive language abilities.
▪ Monitoring for safety
The following measures were adopted to monitor the safety of acupuncture. Parents were advised to directly report possible adverse events as well as acupuncture compliance to the research team or via the Weekly Parental Report; Researchers (including acupuncturist and clinicians) directly observed for adverse events during the acupuncture session.
▪ Statistical analysis
The differences between Pre- and postacupuncture with different outcomes measures (ATEC, PEDI, RDLS, GDDS) were analyzed using the student-t test, Alpha < 0.05 is defined as a significant difference.
Results
▪ Baseline characteristics
Five children with ASD met the inclusion criteria were recruited in current study, with 4 boys and 1 girl, age ranging from 2y to 2y7m. The baseline characteristics of five cases were shown in Table 1, including age, gender, severity of autism, present illness of history, caregivers, use of neuroleptic drugs, whether acupuncture had been received before, received other therapies during acupuncture. All subjects finished all acupuncture sessions.
| Recruited case | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 |
|---|---|---|---|---|---|
| Gender/age | M/2y | M/2y | M/2y6m | F/2y7m | M/2y4m |
| Severity of autism | Severe (CARS=36) | Severe (CARS=36) | Mild-Moderate(CARS=33) | Mild-Moderate (CARS=32) | Mild-Moderate (CARS=32.5) |
| Present illness of history | Social relatedness: Seldom played with peers; poor eye contact; called the name to ignore. |
Social relatedness : Seldom played with peers; poor eye contact; called the name to ignore |
Social relatedness: Less played with peers (with brother sometimes); poor eye contact. |
Social relatedness : Less played with peers; hugged the child when parent asked her to do sometimes; less eye contact; shyness with strangers. |
Social relatedness: Less played with peers (with the older children sometimes); less eye contact. |
| Communication: Shook head for “No” sometimes; without pointing; vocalized “Mum/Dad” non-meaningfully; followed simple commands sometimes. |
Communication: Without pointing; no functional words; followed simple command sometimes |
Communication : Pointing sometimes; shook head for “No”; at 1y6m old, spoke single words (“mum/dad”), followed to call “auntie”, and said “sister” when watched TV; around 2 years old, regression being without functional words; followed simple command sometimes |
Communication : Pointing sometimes; nodded or shook head for “Yes” or “No”; spoke single word (” Mum/Dad”); Reduplication: “chicken” or “duck”; followed simple command sometimes. |
Communication: Pointing sometimes; shook head for “No”; spoke single words (“mum/dad), Reduplication: “Car”; followed simple command sometimes. |
|
| Stereotypic behavior: Hand flicked; body spun; looked at round ball; played wheels of toy car. |
Stereotypic behavior: Hand flicked; body spun; screamed; side head going; licked the smooth plane (glass, computer screen); pulled out father’s armpit hair |
Stereotypic behavior: Pressed switch repeatedly; body spun; licked ground; smelt something in fridge; kept the same road. |
Stereotypic behavior: Sideways glanced; chased shadows; buckled scars; smelt family members’ clothes. |
Stereotypic behavior: Looked at numbers on the car license plate or on the lift; kept the same road; opened and closed door repeatedly. |
|
| Caregivers | Parent | Single father | Parent | Parent /grandparent | Parent |
| Neuroleptic drugs | No | No | No | No | No |
| Acupuncture ever | No | No | No | No | No |
| Other therapies | No | No | No | Special education | No |
Table 1: Baseline Characteristics.
▪ Differences in outcome measures before and after acupuncture
The differences in outcome measures before and after acupuncture assessed by parents (ATEC, PEDI, CGI-I) or by assessor (RDLS, GDDS) were summarized in Table 2. One of parents lost follow-up on the outcomes of ATEC and PEDI. A significant improvement after acupuncture on the developmental quotient (DQ) (p=0.018) of GDDS were detected, which was attributed to the improvements of sub-domains of “Fine Motor” (p=0.016) as well as “Adaptability” (p=0.010) respectively. A non-significant improvements on the “Sociability” domain of ATEC (p=0.05) as well as on the “Self-care” domain of PEDI (p=0.052) were also revealed.
| Baseline | Post-treatment | ||||||
|---|---|---|---|---|---|---|---|
| N | Mean | SD | N | Mean | SD | P value | |
| Autism Treatment Evaluation Checklist (ATEC) | |||||||
| Speech/Language/Communication | 4 | 21.50 | 3.00 | 4 | 20.50 | 5.20 | 0.514 |
| Sociability | 4 | 21.00 | 7.62 | 4 | 16.25 | 9.11 | 0.050 |
| Sensory/Cognitive awareness | 4 | 20.75 | 4.99 | 4 | 19.25 | 3.10 | 0.245 |
| Health/Physical/Behavior | 4 | 22.50 | 8.39 | 4 | 20.00 | 7.75 | 0.141 |
| Total score | 4 | 85.75 | 21.19 | 4 | 76.00 | 19.31 | 0.067 |
| Gesell Developmental Diagnostic Scale (GDDS) | |||||||
| Gross motor | 5 | 93.60 | 6.54 | 5 | 99.40 | 5.41 | 0.205 |
| Fine motor | 5 | 74.00 | 13.13 | 5 | 82.40 | 12.72 | 0.010 |
| Adaptability | 5 | 73.20 | 13.26 | 5 | 83.20 | 17.23 | 0.016 |
| Language | 5 | 40.60 | 9.40 | 5 | 45.40 | 14.59 | 0.376 |
| Personal-Social behavior | 5 | 44.80 | 12.50 | 5 | 47.00 | 12.21 | 0.151 |
| Developmental quotient (DQ) | 5 | 65.20 | 9.99 | 5 | 71.40 | 10.74 | 0.018 |
| Pediatric Evaluation of Disability Inventory (PEDI) | |||||||
| Self-care | 4 | 41.20 | 12.98 | 4 | 45.18 | 12.77 | 0.052 |
| Mobility | 4 | 66.63 | 5.07 | 4 | 67.33 | 6.80 | 0.584 |
| Cognition | 4 | 35.18 | 5.99 | 4 | 37.15 | 8.38 | 0.429 |
| Self-care caregiver assistant | 4 | 24.65 | 22.86 | 4 | 32.93 | 23.06 | 0.214 |
| Mobility caregiver assistant | 4 | 63.60 | 7.64 | 4 | 64.78 | 4.35 | 0.655 |
| Social caregiver assistant | 4 | 26.35 | 18.79 | 4 | 37.58 | 25.08 | 0.127 |
| Reynell Developmental Language Scale (RDLS) | |||||||
| Comprehension (standard score) | 5 | 75.20 | 9.34 | 5 | 77.00 | 11.11 | 0.374 |
| Production (standard score) | 5 | 72.20 | 5.22 | 5 | 74.00 | 6.86 | 0.374 |
| Clinical Global Impression-Improvement (CGI-I) scale | |||||||
| Much improvement | 2 | ||||||
| Minimal improvement | 2 | ||||||
| No change | 1 | ||||||
Table 2: Comparison of Differences in Outcome Measures before and after acupuncture.
▪ Outcomes of weekly parental report
The outcomes of progress of cases reported by parents via Weekly Parental Report were summarized in Table 3.
| Session | Case 1 (M/2y, CARS=36) | Case 2(M/2y, CARS=36) | Case 3 (M/2y6m, CARS=33) | Case 4 (F/2y7m, CARS=32) | Case 5 (M/2y4m, CARS=32.5) |
|---|---|---|---|---|---|
| 1st -5th | Social relatedness | No changes | Communication | No changes | No changes |
| More eye contact; tried to find parent when them in absence (played on his own before); more frequently messed up toys; explored a wider range of environments; used of his butt rubbing parent to cause their attention when sleep together sometimes. | Mouth shapes became more; vocalized more “YiYi” like sound, while pointing to milk; reduplication: “Sister”, “Mother” and “Father” (not done a few months already). | ||||
| Stereotypic behavior/others Less temper tantrum; no longer persistently played ball; Took a candy to eat from drawer; stopped when saw a mouse; held milk bottle with somewhat squeezing actions; put shoes on the ground from shoe case, and wanted to wear by himself; pretended to beating him, he would hide; played saliva sometimes. | Stereotypic behavior/others Had some stereotypic behaviors (biting fingers, knees and hands rubbed ground) |
||||
| 6th -10th | Social relatedness | No changes | Social relatedness | Social relatedness | Communication |
| Eye contact better; responsive to parent’s call, and tried to find them | Played with peers happily sometimes; saw the moon, pointing it to her mother; shook hands with others. | More frequently initiatively pulled other children; more willing to accepting the parent’s hug. | More frequently said single words, such as “sugar”. | ||
| Communication Vocalized more “Mum/Dad”- like or other in-recognizable sounds; scolded by father, tried to find mother and called “mum” clearly; vocalized “you” like sound thrice; followed mother’s order to pass an egg to father. |
Communication More vocalization; more mouth shapes; vocalized “Dada”, “Ah” 及“O”sound; reduplication: “grandma”, “brother” “dad”. |
Communication More vocalization than before. |
Stereotypic behavior/others Read English numbers and letters on the building blocks. |
||
| Stereotypic behavior/others Temper better; “hand flicked” action reduced; imitation improved (listen to the phone; with a cotton ball wiping the skin, like nurse); occupied the bouncy bed, and didn’t let others’ play; built higher building blocks. |
Stereotypic behavior/others Temper tantrum sometimes. |
||||
| 11th -15th | Social relatedness On Middle Autumn Festival: with his parent went into the crowd without fear, happily played , smiled sometimes; wanted to play with two women lying prostrate on the ground, and escaped immediately when found them being in-recognizable. |
No changes | Social relatedness Initiatively applauded after teacher said “good morning”; higher degree of corporation; willing to communicating with others; followed mother’s order to call next door elder sister. |
Social relatedness Looked at mother’s eyes sometimes. |
Communication More vocalizations; said “Car”. |
| Stereotypic behavior/others Mood better; opened the bottle cover, holding it to drink; took his own spoon to eat, and wanted to put the food into his bowl; Took the lantern |
Communication Called brother, grandma, elder sister more frequently; more willing to using language; better comprehension and temper than before; said “Okay” when teacher asked him to find out another teacher; mother asked him to go home, responsive with “Okay” twice. | Communication More vocalization; more frequently followed to say. |
Stereotypic behavior/others Repeatedly opened and closed doors; learned some new letters and words, such as “D, K, J”, “Ball”. |
||
| 16th -20th | Social relatedness Stared at her mother’s classmates and her daughter, with smile, when played with them; watched video with his parent, laughing when saw the funny. |
No changes | Social relatedness Eye-contact better; Initiatively called brother or grandmother in the morning; played with next door elder sister; waited outside door for her to go out, and knocked the door sometimes; not afraid of strangers. |
Social relatedness Initiatively said: “what to do”, “mum ladder”, “mum help”, and mum came”; more frequently initiatively said; hugged other people she liked; kissed others sometimes. |
Social relatedness Initiatively called “dad” or “mum”; initiatively asked mum to do things; Responsive with “A” when called his name. |
| Stereotypic behavior/others He seemed to need parents accompany with him, except listening music. |
Stereotypic behavior/others Took off shoes and gave it to mother; mood more stable. |
Communication More vocalizations; used “no” instead of shaking head; pronunciation and intonation with fluctuation and cadence. |
|||
| Stereotypic behavior/others Identified more building block’s color, though didn’t know how to express. |
Table 3: Progress of Cases as reported by parents during acupuncture course.
▪ Compliance and side-effects
All cases finished all acupuncture sessions, although gentle holding for the child was needed in their initial acupuncture sessions. Initial crying occurred in the first few sessions for some cases, however, all cases adapted easily and tolerated the technique well, with the exception of case 5, in whom, got used to the acupuncture without crying after 5 acupuncture sessions.
Discussion
Severe speech deficit is one of the most debilitating and difficult to treat characteristics of autistic children [24]. The language acquired is related to the prognosis of the autistic patients, because in the learning, self-support, social networking, and community participation, verbal ability is a decisive tool. The dysfunction of mirror neuron system (MNS) and its related networks are considered to associate with autism communication, social and emotional regulation [6]. Recent research has shown that representations of the mirror neurons can be altered by training [11].
Acupuncture making is one possible medium through which the putative MNS can be engaged into. In traditional Chinese acupuncture, nearly 400 acupoints on the body surface are interrelated to various functions. The surface acupoints were linked through 14 meridians to various organs or viscera of the human body. According to Traditional Chinese Medicine (TCM) philosophy, health is achieved by maintaining an uninterrupted flow of “Qi” along 14 meridians throughout the body. Disease is caused by stagnation to the flow of this “Qi” or energy [25]. Acupuncture could help to restore the smooth flow of Qi, thus restoring the internal balance [25].
The TCM approach for Autism spectrum disorder (ASD) is more holistic [26]. The pathogenesis of autism is the derangement and insufficiency of the Brain and Mind [26]. Previous randomized controlled trial (RCT) showed that a short course of electro-acupuncture was useful to improve specific functions in children with ASD, especially for language comprehension and self-care ability [27], while another RCT study reported that scalp acupuncture was a safe complementary modality when combined with language therapy and had a significant effect on language development in children with ASD [28]. Recent animal study also reported that laser acupuncture could improve autistic-like behaviors and brain oxidative stress status in the valproic acid rat model of autism [29], while another study postulated that the potential therapeutic effect of acupuncture-induced activation of BDNF in the treatment of ASD [30]. The aim of current study was to explore the efficacy and safety of acupuncture specifically for non-verbal autistic children.
Based on the philosophy of TCM, the selected two acupoints in current study are located in the Hand Foot Shaoyang meridian, which have the characteristics of germinal life and growth in nature. The rationale of intervention on selected acupoints was to germinate Qi and dredged Qi of the liver and bile meridian, benefiting brain function accordingly.
There is a close relationship between the nervous system and the acupoint [31]. It is assumed that a continuous neurological response will be triggered by the fine needle insertion of these nerves, which can be happen similar to the local or local implementation, or distant [32]. In the central nervous system, it is mainly mediated by sensory nerve to many structures, which can lead to the activation of the pathway and affect the various physiological systems of the brain and the surroundings [33]. Presumptively, there might anatomically (Figure 1) be a close relationship between the selected acupoints [the temporal anterior oblique (MS6) under 2/5 and temporal posterior oblique (MS7) under 2/5] and the jacent center nervous systems including the Broca area and superior temporal sulcus (both containing MNS). Therefore, acupuncture intervention may be indirectly engaged into MNS, and consequently improved the social relatedness, communication as well as related symptoms of non-verbal autistic children, via modifying the dysfunctional MNS accordingly.
Research has demonstrated a relationship between joint attention and language development in children with autism. One of the strongest predictors for subsequent language acquisition and expressive language abilities was responsiveness to bids for joint attention at initial assessment [34]. Interestingly, joint attention was improved in some cases in current study, e.g. Case 3 pointed to moon for her mother (Table 3), in accordance with non-significant improvement of the “sociability” domain of ATEC (p=0.05) (Table 2). Imitation is also considered to be a precursor of language development [35]. The improvements of the imitation ability were also noted in Case 1 (e.g. listened to the phone, used a cotton ball wiping the skin), as well as in Case 4 with imitating others to say more (Table 3).
The presence of cognitive impairments is also assumed to play pivotal roles in poor language acquisition [4]. There was a significant improvement in the developmental quotient (DQ) (p=0.018) (Table 2) of cases after acupuncture, in accordance with the improvement of outcomes of Weekly Parental Report in some cases, e.g. Case 1 took a candy from drawer to eat; Case 4 identified more building blocks’ color (Table 3). Furthermore, the improvement of DQ was attributed to the significantly ameliorated in sub-domains of “fine motor” (p=0.010) and “adaptability” (p=0.016) (Table 2), in coincided with the outcomes of Weekly Parental Report, with the improvement of “fine motor” skill, e.g. Case 1 built higherlevel building blocks and took his own spoon to eat; Case 4 took off shoes and delivered them to her mother, as well as the improvement of “imitation” skill as described above (Table 3). The “imitation” skill tests are included in the “adaptability” domain of GDDS accordingly.
The improvements of communication were noted according to the outcomes of Weekly Parental Report, although there were no significant changes in the domain of Speech/ Language/Communication of ATEC and the outcomes of RDLS either in Comprehension or Production domain. Specifically, some evident changes were found in some cases e.g. called “mum” appropriately first time in Case 1, said “no” instead of shaking head in Case 4, and said “sugar” in Case 5 (Table 3); regarding receptive communication, Case 3 could answer “OK”, when mother asked him to return home; moreover, Case 5 could reply “Yes” when his father called his name, and Case 1 could pass the egg to his father when mother asked him to do so (Table 3).
The idea of a mirror-like system in language processing was first assumed in the “motor theory of speech perception” [36]. According to this theory, speech perception relies strongly on observation of the articulatory (motor) gestures of the speaker (e.g. movements of the mouth, lips, and tongue), rather than the acoustic cues of speech sounds [11]. To successfully process spoken language, these motor actions must be represented in the listener’s brain, so that the regions critical to speech production also become activated when the listener sees articulatory gestures [11]. Interestingly, the case 3 showed more mouth shapes and wanted to vocalize (Table 2). Furthermore, more intonation in fluctuation and cadence in Case 4 were also reported.
Some stereotyped behaviors were improved in some cases based on the outcomes of Weekly Parental Report (Table 2), e.g. less compulsive behaviors in Case 1 (no longer persistently played ball; reduced the “flicking” action). However, some stereotypic behaviors were also reported in Case 5 (repeatedly opened and closed door) and in Case 3 (knees and hands rubbed ground) at initial acupuncture sessions, although both disappeared in the soon later sessions (Table 2).
In terms of the functional status, the much improvement of CGI-I in Case 1 on the the domains of “social relatedness and imitation,” as well as in Case 3 on the “social relatedness, verbal and non-verbal communication” domains were found, while minimal improvement of CGI-I on the domain of “Social relatedness and Communication” was also detected in Case 4 and Case 5 (Table 3). No changes were reported in Case 2. The non-significant improvements (p=0.052) on the “self-care” domain of PEDI were also revealed (Table 3).
Children with ASD may experience adverse effects of acupuncture but are unable to convey relevant information to their parents or the researchers due to the impairment of communication [26]. The definition of “acupuncture compliance” is that subjects were able to sit or lie on a couch to accept acupuncture, even if they cried or needed gentle hand or head holding [27]. Good compliance was defined as being able to accomplish this within the first three sessions [27]. All cases in current study accepted acupuncture first time, and had a good compliance, with the exception of Case 5, who tolerated the technique well after 5 acupuncture sessions.
Although the improvements in some core features, and some related domains (cognition and imitation) of non-verbal autistic children were detected in current pilot study, there were some precautions in order to avoid misinterpreting the outcomes. First, this pilot study is a small case series including only 5 cases. Secondly, the symptoms of young subjects (2y~2y7m) might improve automatically even in the short time period (4 weeks) due to the developmental processes in nature. Thirdly, the statistically significant results should be carefully interpreted as relatively comprehensive assessment tools included in current study, which might easily cause false positive outcomes. Fourthly, except for the “Sociability” and “cognitive” domains, the improvement of communication domains and stereotypic behaviors were mostly supported by Weekly Parental Report, rather than the standard assessment scales such as ATEC.
In sum, a short intensive course of acupuncture for the selected acupoints might improve some core features of children with non-verbal ASD. Based on the outcomes of pilot study, we had performed a randomized controlled trial to further study the efficacy and safety of acupuncture for non-verbal autistic children, and also explored the changes of neurochemical substrates, via modern neuroimaging technique.
Funding Source
This research is supported by the grants of Science and Technology Department of Guangdong Province of China (2013B021800046) and and Wen-Xiong Chen’s Doctoral Fund of Guangzhou Women and Children’s Medical Center (5001-2170057).
Conflict of Interest
There are no conflicts of interest for all authors in this study.
Author Contributions
CWX and LG conceptualized the study. CWK designed the study. LG performed acupuncture. CWX and HZF recruited and assessed the subjects. CWX analyzed the data and drafted the manuscript. LHS and ZSH performed MR. All authors have agreed on the final version.
Acknowledgments
We would like to thank all of the participants who participated in this study.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Arlington (VA): American Psychiatric Publishing (2013).
- Tager-Flusberg H. Language and understanding minds: connections in autism. In: Baron-Cohen S, Tager-Flusberg H, Cohen DJ. Understanding other minds: Perspectives from autism and developmental cognitive neuroscience. Oxford:Oxford University Press, 124-149 (2000).
- Volkmar FR, Lord C, Bailey A, et al. Autism and pervasive developmental disorders. J. Child. Psychol. Psychiatry 45(1), 135-170 (2004).
- Venter A, Lord C, Schopler E. A follow-up study of high-functioning autistic children. J. Child. Psychol. Psychiatry 33(3), 489-507(1992).
- Rogers SJ, Hayden D, Hepburn S, et al. Teaching young nonverbal children with autism useful speech: A pilot study of the Denver model and PROMPT interventions. J. Autism. Dev. Disord 36(8), 1007-1024 (2006).
- Baron-Cohen S, Leslie AM, Frith U. Does the autistic-child have a theory of mind? Cognition 21(1), 37-46 (1985).
- Barsalou LW. Perceptual symbol systems. Behav. Brain. Sci 22(4), 577-609 (1999).
- Gangitano M, Mottaghy FM, Pascual-Leone A. Phase-specific modulation of cortical motor output during movement observation. Neuroreport 12(7), 1489-1492 (2001).
- Buccino G, Lui F, Canessa N, et al. Neural circuits involved in the recognition of actions performed by nonconspecifics: an fMRI study. J. Cogn. Neurosci 16(1), 114-126 (2004).
- Baumann S, Koeneke S, Schmidt CF, et al. A network for audio-motor coordination in skilled pianists and non-musicians. Brain. Res 1161, 65-78 (2007).
- Wan CY, Demaine K, Zipse L, et al. From music making to speaking: Engaging the mirror neuron system in autism. Brain. Res. Bull 82(3-4), 161-168 (2010).
- Adams D, Dagenais S, Clifford T, et al. Complementary and alternative medicine use by pediatric specialty outpatients. Pediatrics 131(2), 225-232 (2013).
- Brondino N, Fusar-Poli L, Rocchetti M, et al. Complementary and alternative therapies for autism spectrum disorder. Evid. Based. Complement. Alternat. Med 258589 (2015).
- Cheuk DKL, Wong V, Chen WX. Acupuncture for autism spectrum disorders (ASD). Cochrane. Database. Syst. Rev (9), CD007849 (2011).
- Yang CS, Hao ZL, Zhang LL, Guo Q. Efficacy and safety of acupuncture in children: an overview of systematic reviews. Pediatr. Res 78(2), 112-119 (2015).
- Schopler E, Reichler RJ, Renner BR. The Childhood Autism Rating Scale (CARS) for Diagnostic Screening and Classification in Autism. New York: Irvington Publishers (1986).
- Lord C, Rutter M, Le Couteur A. Autism Diagnostic Interview-Revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J. Autism. Dev. Disord 24(5), 659-685 (1994).
- Lord C, Rutter M, DiLavore PC. Autism Diagnostic Observation Scale-Generic. Chicago: University of Chicago Press (1997).
- Rimland B, Edelson M. Autism Treatment Evaluation Checklist. SanDiego: Autism Research Institute (1999).
- Haley SM, Coster WJ, Ludlow LH, et al. Pediatric Evaluation of Disability Inventory: Development, standardization, and administration manual, Version 1.0. Boston MA: PEDI Research group (1992).
- No authors listed. Rating scales and assessment instruments for use in pediatric psychopharmacology research. Psychopharmacol. Bull 21(4), 714-1124 (1985).
- Gesell A, Amatruda CS, Knobloch H, et al. Gesell and Amatruda’s Developmental Diagnosis: the Evaluation and Management of Normal and Abnormal Neuropsychologic Development in Infancy and Early Childhood. New York:Harper and Row (1974).
- Reynell JK, Gruber CP. Reynell Developmental Language Scale. Los Angeles: Western Psychological Services (1990).
- Rutter M. Diagnosis and definition. In: Rutter M, Schopler E. Autism, a reappraisal of concepts and treatment. New York: Plenum Press, 1-25 (1978).
- Wong V, Chen WX. Is acupuncture useful for cerebral palsy? What evidence do we have? In: Fong HD. Trends in cerebral palsy research. New York: Nova Science Publishers Inc, 139-165 (2005).
- Chen WX, Wong V, Liu WL. Electroacupuncture for children with autism spectrum disorder: Pilot study of 2 cases. J. Altern. Complement. Med 14(8), 1057-1065 (2008).
- Wong V, Chen WX, Liu WL. Randomized Controlled Trial of electro-acupuncture for autism spectrum disorder. Alter. Med. Rev 15(2), 136-146 (2010).
- Allam H, Eldine NG, Helmy G. Scalp acupuncture effect on language development in children with autism: a pilot study. J. Altern. Complement. Med 14(2), 109-114 (2008).
- Khongrum J, Wattanathorn J. Laser acupuncture improves behavioral disorders and brain oxidative stress status in the valproic acid rat model of autism. J. Acupunct. Meridian. Stud 8(4), 183-191(2015).
- Li LY, Jiang N, Zhao Y. Could acupuncture have a role in the treatment of autism spectrum disorder via modulation of BDNF expression and activation? Acupunct. Med 32(6), 503-505 (2014).
- Fu H. What is the material base of acupuncture? The nerves! Med. Hypotheses 54(3), 358-359 (2000).
- Jansen G, Lundeberg T, Kjartansson J, et al. Acupuncture and sensory neuropeptides increase cutaneous blood flow in rats. Neurosci. Lett 97(3), 305-309 (2000).
- Johansson K, Lindgren I, Winder H, et al. Can sensory stimulation improve the functional outcome in stroke patients? Neurology 43(11), 2189-2192 (1993).
- Sigman M, Ruskin E, Arbeile S, et al. Continuity and change in the social competence of children with autism, Down syndrome, and developmental delays. Monogr. Soc. Res. Child. Dev 64(1), 1-114 (1999).
- Hadjikhani N. Mirror neuron system and autism. In: Carlisle PC. Progress in autism research. New York:Nova Science Publishers Inc, 151-166 (2007).
- Liberman AM, Mattingly IG. The motor theory of speech perception revised. Cognition 21(1), 1-36 (1985).