Case Report - (2020) Volume 10, Issue 5
A Survivor of a Motor Vehicle Accident with Depression and Cognitive Impairment a Case of Probable Creutzfeldt - Jakob disease
Mason Chacko 1,2,*, JeissonFontecha-Hernandez1, Jessica Carbajal1, Robert Peyeser1, Ricardo Cáceda1,3
1Department of Psychiatry, Stony Brook University, Stony Brook, New York, USA
2Department of Hospital Medicine, South Shore University Hospital, Bay Shore NY USA
3Psychiatry Service, Northport VA Medical Center, Northport, New York, USA
*Corresponding Author: Mason Chacko
Department of Psychiatry, Stony Brook University HSC T10-020
Stony Brook, NY, 11794
Tel: 631-638-1538
Fax: 631-444-1560
E-mail: [email protected]
Abstract
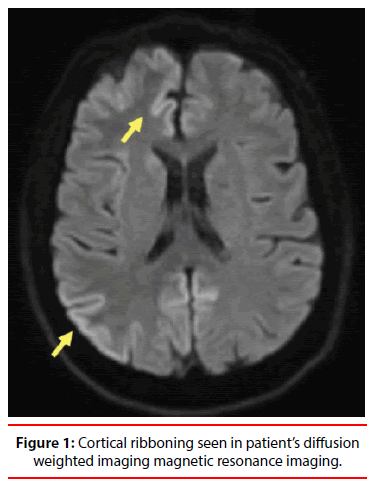
Introduction: Creutzfeldt-Jakob disease (CJD) is a lethal prion disease which can present with a variety of neurological or psychiatric presentations. Even though the outcome is eventually lethal, CJD can be unrecognized and confuse prognosis and management. Case Presentation: We present a case of a 65-year old female with history of depression and anxiety who presented following a motor vehicle accident, confused, tongue deviation, vertical nystagmus, and with history of progressive lapses in memory. After initial work up, she was diagnosed with probable CJD based on cortical ribboning in diffusion weighted imaging magnetic resonance imaging, a positive cerebrospinal fluid 14-3-3 protein and vertical nystagmus supported the diagnosis of probable CJD. Conclusions: We add to the nascent literature by presenting a case of probable CJD with an initial atypical presentation of depression, anxiety and memory impairments.
Keywords
Depression, Cognitive Impairment, Creutzfeldt - Jakob disease
Introduction
Creutzfeldt-Jakob disease (CJD) is a lethal prion disease, classified among the infectious encephalopathies. Although most cases are sporadic, it can have a genetic component or transmitted through a variety of routes, including ingestion of infected meat products. The global incidence of CJD is approximately one per million individuals per year [1]. CJD is an uncommon cause of dementia, but must be considered as a differential diagnosis in the context of rapid onset cognitive decline, suggestive electroencephalography (EEG) or imaging findings. As a prion disease, CJD demonstrates unique findings: neuronal loss in gray matter leads to appearance of vacuoles in the neuropil creating a “sponge-like” appearance. We present a patient with initial presentation with major depression and cognitive decline, who was finally diagnosed with probable sporadic CJD based upon history, physical findings and neuroimaging.
Case Presentation
A sixty-five-year-old married Hispanic female with history of hypertension, hyperlipidemia, anxiety and depression presented to the Emergency Department (ED) after she struck a utility pole while driving her car. She was found to have right sided tongue deviation and vertical nystagmus. Her blood pressure was 205/110 and she was started on cardene drip for optimal blood pressure control. Her blood count and metabolic profile were unremarkable. A noncontrast head computerized tomography showed no acute intracranial pathology.
She was hospitalized for further work up and to rule out an ischemic cause. She underwent electroencephalography (EEG) which showed generalized background slowing, right hemispheric skewing and abnormal focal cerebral dysfunction which was suggestive of possible seizure activity. An initial non-contrast magnetic resonance imaging (MRI) showed a possible subarachnoid hemorrhage, but a repeat MRI with diffusion weighted imaging (DWI) showed no subarachnoid hemorrhage but bilateral occipital and temporal enhancement of unknown etiology. The cardene drip was continued for treatment of hypertensive encephalopathy. The patient’s family reported her having difficulty with short term memory, for example as a bus driver she recently drove her vehicle to the wrong station. They also reported ataxia and unsteady gait, as well as depressed mood, insomnia, 10-pound weight loss, severe anhedonia, abulia and psychomotor retardation for the past eight weeks.
After three days in the Medicine ward, her symptoms improved and Psychiatry was consulted at the request of her husband for worsening of depressive symptoms. On the initial psychiatric evaluation, she was found to be isolative with flat affect and to have intermittent anomic aphasia. Sporadic “lower extremity shaking” was also noted and continued on follow up visit. This later would prove to be myoclonic in nature and remained intermittent throughout the patient hospitalization. Prior to admission the patient was on escitalopram 10 mg daily, sertraline 50 mg daily, and had been recently started on alprazolam 0.5 mg three times a day as needed by her primary care physician for worsening anxiety. Primary care team was advised to continue sertraline, discontinue escitalopram and taper alprazolam in the setting of cognitive decline. Patient scored nine on the Beck Depression Inventory. The DWI MRI was reviewed with a neuro-radiologist and cortical ribboning was noted (Figure 1), which was indicative of early prion disease. Obtaining additional history, the patient was American born, had lived all her life in urban settings, with no prior surgeries or international travel. In the setting of depression, rapid cognitive decline and focal neurological findings, a sonogram guided lumbar puncture was performed to rule out infectious or inflammatory conditions. The patient was subsequently discharged to subacute rehabilitation pending results. The cerebrospinal fluid (CSF) revealed normal protein, glucose and electrolyte levels but marked elevation of 14-3-3 protein levels (12,242 pg/ml).
Cortical ribboning in DWI MRI, a positive CSF 14-3-3 protein with vertical nystagmus supported the diagnosis of probable CJD. The MRI films were sent to the Foundation InstitutoNeurologicoBesta in Milan, Italy for diagnostic consultation, which confirmed radiological findings consistent with CJD. The patient was transferred to a subacute rehabilitation facility. However, she showed failure to thrive, with progressive neurological decline and was re-hospitalized two weeks later for generalized seizures. She entered into inpatient hospice care and expired within the week.
Discussion
CJD is a fatally progressive prion disease characterized by progressive dementia. The sporadic form is seen in 87% of the cases. Of the remaining cases and less than 1% is iatrogenic. Familial CJD is associated with relatively early disease onset, usually between the ages of 40-50 years. In contrast, sporadic CJD usually presents between the ages of 50-70 years of age and is characterized by a rapidly progressive dementia and myoclonus. Given the relatively low prevalence of CJD, keeping CJD in mind as part of the differential diagnosis may help to increase its detection in cases of dementia with atypical presentation [2]. The psychiatric manifestations include mood, psychosis, agitation and insomnia. The depressive symptoms occur early, whereas psychotic symptoms appear in later stages of the disease. The most common symptoms are changes in sleep patterns (approximately in of 50% cases) [3]. Approximately 40% of patients show mood symptoms at any point during the disease [3]. The most common depressive symptoms include decreased appetite, weight loss, anhedonia and feelings of guilt. Even though psychotic symptoms become more prevalent as the disease process advances, approximately 20% of CJD patients present with at least one psychotic symptom [4]. Disorganized thoughts, perseveration and confabulation occur in approximately 25% of patients, while agitation occurs even more frequently (30% of the time) [3]. Bizarre behaviors and episodes of wandering are seen less often.
Remarkably, despite occurring early in more than 40 % percent of cases, mood and anxiety symptoms are not part of the diagnostic criteria for CJD. The late life onset of depressive symptoms in the context of cognitive impairment and new neurological symptoms, particularly myoclonus, should warrant raising the suspicion of rarer etiologies like spongiform encephalopathies and other rare organic causes. Patients who present with altered mental status, depression and anxiety should undergo complete workup which includes complete blood count, complete metabolic profile, urine analysis, liver function tests including ammonia level and EEG. A lumbar puncture along with radiological imaging should be pursued in the setting of acute changes in cognition and sensorium.
There are no curative treatments for CJD, which is unvaryingly fatal. Comfort measures and psycho-education for patients and their families can be beneficial, in particular support regarding what to expect and advanced directives. Even though most symptoms of prion disease result from the irreversible loss of brain function and do not resolve once they have appeared, psychiatric symptoms tend to fluctuate and there may be room for pharmacological interventions [3,5]. Various classes of antidepressants have been used but none appeared to be effective in patients with CJD (Zerr and Poser 2002) The use of antipsychotic drugs has shown some benefits in addressing hallucinations and agitation [4]. Lorazepam and other short acting benzodiazepines are valuable alternatives for anxiety and agitation in patients with CJD. Memantine, has demonstrated small therapeutic benefits in tissues and rodent models [6].
The average course of CJD lasts approximately one year. In this case report, the patient’s symptoms of progressive deterioration in cognition, myoclonus along with positive neuroimaging and serum markers were consistent with probable sporadic CJD. Although there is no effective treatment of CJD, current approaches include supportive care and symptomatic management focusing on agitation and sleep. Patients may require intensive care admission in the acute setting and then may be transitioned to comfort care measures.
Disclosure Statement
The authors declare nothing for disclosure
Acknowledgements
None
References
- Mackenzie G, Will R. (2017) Creutzfeldt-Jakob disease: recent developments. F1000Res 6(1): 2053.
- Xu Y, Xu J, Zhang J, Cai Z, Wei H, et al. (2019) Sporadic Creutzfeldt-Jakob disease presenting as dizziness and cognitive decline: A case report. Medicine. (Baltimore) 98(24): e16002.
- Wall CA, Rummans TA, Aksamit AJ, Krahn LE, Pankratz VS. (2005) Psychiatric manifestations of Creutzfeldt-Jakob disease: a 25-year analysis. J. Neuropsychiatry. ClinNeurosci 17(4): 489-495.
- Zerr I, Poser S. (2002) Clinical diagnosis and differential diagnosis of CJD and vCJD. With special emphasis on laboratory tests. APMIS 110(1): 88-98.
- Riemer C, Burwinkel M, Schwarz A, Gültner S, Mok SWF, et al. (2008) Evaluation of drugs for treatment of prion infections of the central nervous system. J Gen Virol 89(2): 594-597.
- Müller WE, Ushijima H, Schröder HC, Forrest JM, Schatton WF, et al. (1993) Cytoprotective effect of NMDA receptor antagonists on prion protein (PrionSc)-induced toxicity in rat cortical cell cultures. Eur J Pharmacol 246(3): 261-267.