Case Report - Neuropsychiatry (2017) Volume 7, Issue 6
A Rare Case of Cryptococcus Meningoencephalitis Presenting with Acute Brainstem Infarction in an Immunocompetent Host
- Corresponding Author:
- Fu-Chi Yang, MD, PhD
Department of Neurology, Tri-Service General Hospital, National Defense Medical Center, No. 325, Section 2, Cheng-Kung Road, Neihu 114, Taipei, Taiwan, Republic of China
Tel: +886 2 87923311 Ext: 88078
Fax: +886 2 87927174
Abstract
Abstract
Background: Cryptococcal meningitis (CM) occurs most commonly in immunocompromised patients. Here, we report a rare case of CM in an immunocompetent patient who presented with an acute stroke.
Case report: A 60-year-old woman came to our hospital with complaints of dizziness, dysarthria, and a right side-deviated gait. A head computed tomography (CT) showed a low-density lesion in the left caudate, consistent with recent infarction. Within a day of admission, she developed headache, fever, and a mild Brudzinski’s sign. Magnetic resonance imaging showed an acute lacunar infarct in the left midbrain as well as vasogenic edema in the left caudate head and left genu of the corpus callosum. A cerebrospinal fluid (CSF) examination showed elevated opening pressure, a high white blood cell count, a low glucose level, and a high protein level. CSF pathology revealed Cryptococcus neoformans yeast cells and C. neoformans was cultured from a CSF sample. The patient was treated with curative antifungal and prophylactic antiplatelet medications and recovered without long-term sequelae.
Conclusion: CM should be considered as a differential diagnosis in acute stroke patients with fever and potential pathogen-contact history, even if they are non-immunocompromised. Missed CM diagnosis can result in inappropriate management, affecting the patient’s clinical outcome.
Keywords
Cryptococcus meningitis, Stroke, Cerebrospinal fluid, Immunocompetent
Introduction
Opportunistic yeast infections of the central nervous system (CNS) are frequently caused by Cryptococcus fungi [1]. Immunocompromising conditions that leave patients at risk of cryptococcal CNS infections include HIV infection, leukemia, post-transplantation immunosuppression, an organ failure syndrome, or innate immunologic problems, such as common variable immunodeficiency [2,3]. Fungal infections of the CNS can manifest as meningitis, abscesses, granulomas, or infarction [4]. Cryptococcal meningitis (CM), the most common manifestation of cryptococcosis among patients with impaired cell-mediated immunity, is caused by the encapsulated yeast organism Cryptococcus neoformans.
Stroke can arise as a complication of CM. It is not standard practice to examine the cerebrospinal fluid (CSF) of stroke patients. However, the identification of a cryptococcal pathogen in CSF can guide therapeutic choices in patients who have suffered an arterial stroke secondary to CM [2].
Cryptococcal infection involving the CNS in non-immunocompromised patients is uncommon and presents unique diagnostic and therapeutic challenges. Detailed literature addressing the distinctions between CM in immunocompromised versus immunocompetent patients is lacking [3]. To our knowledge, there have been only few reports of acute onset hemiparesis in a patient with CM [4]. Here, we describe the case of an otherwise healthy female patient diagnosed with CM presenting with acute infarction.
Case Report
A 60-year-old woman came to our hospital’s emergency department complaining that she had awoken with dizziness, dysarthria, and a right side-deviated gait. She indicated that she had been experiencing a severe headache and mild fever for several days. She reported that she had had a bicycle accident that resulted in multiple abrasions on her right arm and leg. The patient had a history of hypertensive cardiovascular disease and gastric ulcers, which had been controlled by medication for several years. She denied smoking, alcoholism, or any recreational drug abuse.
The patient’s initial emergency department examination revealed a normal pulse rate (79/ min), blood pressure (130/90 mmHg), and temperature (37.2°C). She was alert and welloriented with coherent albeit dysarthric speech. Her pupil diameters were symmetrically 3 mm and responded normally to light. Cranial nerve examination revealed a freely conjugated gaze without nystagmus and a flattened right nasolabial fold. Her corneal, oculocephalic, and gag reflexes were intact. She had mild right hemiparesis and normal sensory function. Her biceps, triceps, knee, and ankle reflexes were symmetrical with bilateral plantar flexor responses. Her motor coordination was smooth. An electrocardiogram showed a sinus rhythm and chest radiography showed a tiny nodular opacity in the right lower lung. Computed tomography (CT) showed a low-density lesion in the left caudate nucleus head region, consistent with a recent brain infarction. The patient was admitted for further observation.
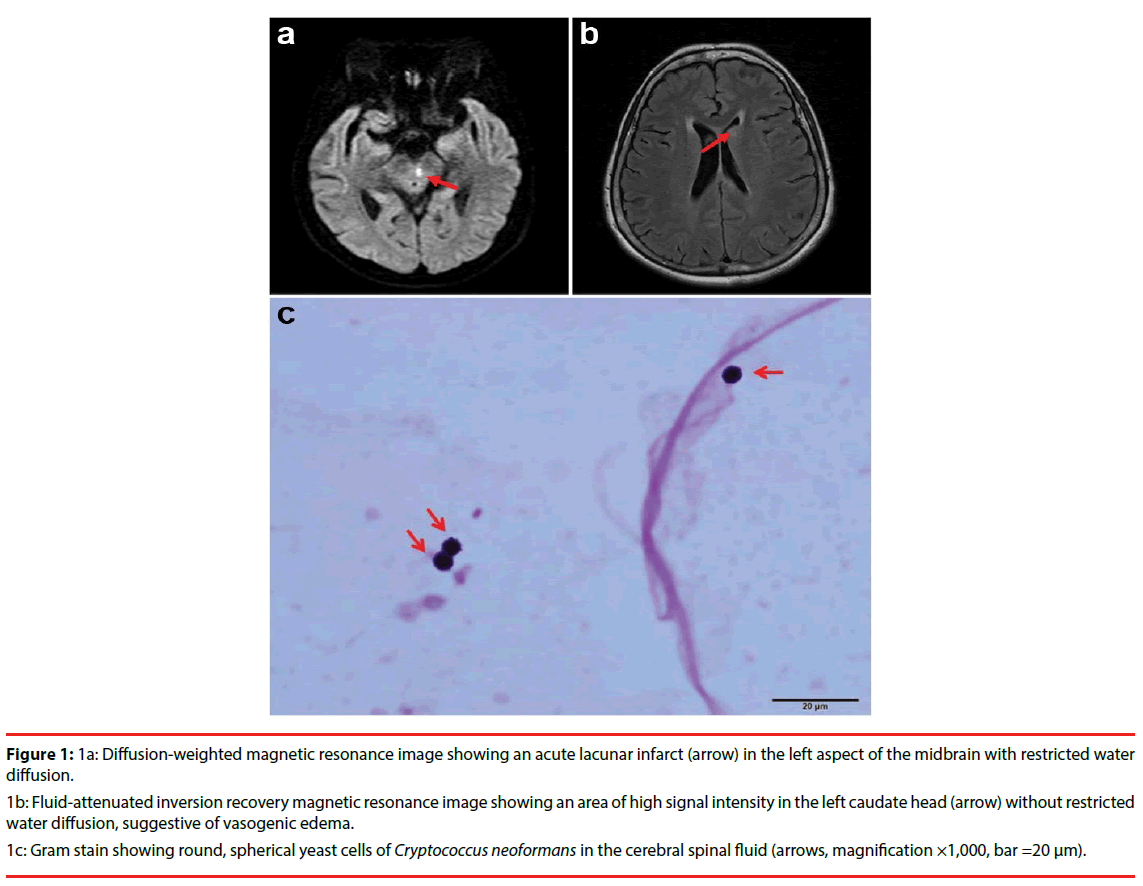
The next day, the patient had a bilateral temporal dull headache with a fever (38.9°C), and exhibited a mild Brudzinski sign. Brain magnetic resonance imaging showed an acute infarction in the left midbrain (Figure 1a) with vasogenic edema in the left caudate head (Figure 1b) and the left aspect of the genu of the corpus callosum. The magnetic resonance angiography was normal. Blood tests indiated that the patient had normal immunological function and HIV antibody-negative serum. A lumbar puncture and CSF analysis showed elevated opening pressure (25 cmH2O), a high white blood cell count (156 leukocytes/μL), a low CSF glucose level (15 mg/dL), and a high CSF protein level (144 mg/dL). Upon finding these signs of possible CNS infection, the patient recalled that she had been in contact with pigeon excreta in her neighborhood. Subsequent CSF pathology revealed the presence of spherical C. neoformans yeast cells. C. neoformans was cultured from a CSF sample (Figure 1c), and the cryptococcal antigen titer was 1:4. CT examinations were performed to gain further information about the nodular opacity in the patient’s right lower lung and for evaluation of possible systemic cryptococcosis. Chest CT showed one nodular opacity (~0.4 cm in diameter) and suspected inflammatory, Abdominal CT revealed some hepatic cysts and bilateral renal cysts. No clear evidence of systemic cryptococcosis was obtained.
Figure 1: 1a: Diffusion-weighted magnetic resonance image showing an acute lacunar infarct (arrow) in the left aspect of the midbrain with restricted water diffusion.
1b: Fluid-attenuated inversion recovery magnetic resonance image showing an area of high signal intensity in the left caudate head (arrow) without restricted water diffusion, suggestive of vasogenic edema.
1c: Gram stain showing round, spherical yeast cells of Cryptococcus neoformans in the cerebral spinal fluid (arrows, magnification ×1,000, bar =20 μm).
The patient was treated successfully with intravenous amphotericin B (0.5 mg/kg per day) and oral flucytosine (37.5 mg/kg every 6 hours) for 6 weeks. Aspirin was prescribed for stroke prevention, and soon replaced with ticlopidine due to aspirin-related epigastric discomfort. She was prescribed fluconazole (400 mg/day) as a consolidation therapy for the next 2 weeks, and maintained on low-dose fluconazole (200 mg/ day) therapy thereafter. At the conclusion of her consolidation therapy, the patient was discharged with minor neurological sequelae with slight weakness in her left limbs. The patient has shown no signs of neurological sequelae in over 3 months of follow-up.
Discussion
In the present case, CM comorbid with an acute infarct was discovered in an immunocompetent patient. Previous reports regarding to immunocompetent patients presenting with acute cerebral infarction and concomitant CM were scarce. Most of these cases with acute ischemic stroke and simultaneous CM were susceptible to CNS infections because of certain conditions, including AIDS, diabetes mellitus, post-transplantation, and use of immunosuppressants, organ failure syndrome, and occult malignancies [5]. Another case of cryptococcal meningoencephalitis and focal cerebral vasculitis in a 60-year-old woman, while low OKT4 lymphocytes level of 6% (absolute number: 70) was identified [6]. The authors could not determine whether the immunodeficiency favored cryptococcal meningoencephalitis or appeared as a consequence of it [6]. Both cases possessed immunocompromising factors. Furthermore, 3 cases of otherwise healthy patients with acute ischemic stroke and simultaneous cryptococcal meningitis were previously reported [4,7,8]. These cases were similar to our case that no potential immunocompromising conditions were documented after intensive investigations.
The presentation of CM in immunocompetent patients resembles that in HIV-positive hosts in that, relative to immunocompromised patients with CM, immunocompetent hosts often show a relatively acute onset of signs and symptoms, lower positive India ink stain rates, lower CSF antigen titers (<1:1,024), higher CSF host cell counts, less frequent cryptococcosis or extracranial involvement, fewer parenchymal brain lesions, and lower intracranial pressure. Common manifestations of CNS cryptococcosis include intracranial hypertension and basilar meningitis. Our patient presented with an uncommon CM complication, namely stroke due to vasculitis; other uncommon complications of CM include hydrocephalus and subdural fluid accumulation [8].
When chronic meningitis is comorbid with infarction, infarctions are usually located in the basal ganglia, internal capsule, or thalamus, and are rarely found in the brain stem or major vascular territories. Several pathophysiologic mechanisms have been proposed in the development of cerebral infarctions in meningitis, including: (i) vasculitis of vessels that transverse the exudates at the base of the brain, resulting in inflammation-induced spasms, constriction, and thrombosis; (ii) meningeal inflammatory exudate involving the adventitia that spreads progressively until it affects the entire vessel wall, leading to necrotizing panarteritis with secondary thrombosis and occlusion; and (iii) dilated ventricles stretching an already-compromised vessel [9].
With the availability of highly sensitive imaging techniques, CSF analyses are not commonly performed. Nonetheless, CSF analysis may be useful in cases of apparent ischemic stroke due to discrete or occult infectious and inflammatory processes, which tend to involve intracranial arteries. The presence of yeast cells of variable sizes with a thick capsule and narrow-based budding in CSF pathology is virtually diagnostic of CM [2].
Conclusion
Clinical physicians should be alerted to CM as a rare but possible fever etiology in acute stroke patients, even if the patients are immunocompetent. For acute stroke patients presenting to the emergency department with fever, careful documentation of contact history and CSF studies are warranted. More thorough assessments including additional laboratory and radiological tests may also be necessary. Failure to recognize the early clinical manifestations of CM may lead to a markedly delayed diagnosis, inappropriate treatment, and deterioration of prognosis in otherwise healthy patients [10]. Ultimately, a missed CM diagnosis can result in severe neurological disability or even death. Hence, it is important to consider fungal infections in the differential diagnosis of stroke in immunocompetent patients.
Declaration of interests
The authors report no conflicts of interest.
Acknowledgments
This project was supported in part by grants from the Ministry of Science and Technology of Taiwan (MOST 105-2314-B-016-004-); Tri-Service General Hospital, Taiwan (TSGH-C101-159, and TSGH-C106-068)
References
- Fugate JE, Lyons JL, Thakur KT, et al. Infectious causes of stroke. Lancet. Infect. Dis 14(9), 869-880 (2014).
- Cachia D, Singh C, Tetzlaff MT, et al. Middle cerebral artery territory infarct due to Cryptococcus infectionstitle. Diagn. Cytopathol 43(8), 632-634 (2015).
- Pappas PG. Cryptococcal infections in non-HIV-infected patients. Trans. Am. Clin. Climatol. Assoc 1249(1), 61-79 (2013).
- Kalita J, Bansal R, Ayagiri A, et al. Midbrain infarction: a rare presentation of cryptococcal meningitis. Clin. Neurol. Neurosurg 101(1), 23-25 (1999).
- Hayes L, Malhotra P. Central nervous system infections masquerading as cerebrovascular accidents: Case series and review of literature. IDCases 1(4), 74-77 (2014).
- Scalzini A, Castelnuovo F, Puoti M, et al. A case of cryptococcal meningoencephalitis and focal cerebral vasculitis with transient immunodeficiency. Acta. Neurol (Napoli) 12(1), 301-304 (1990).
- Tyler KL, Johnson ECB, Cantu DS, et al. A 20-Year-Old Woman with Headache and Transient Numbness. Neurohospitalist 3(2), 101-110 (2013).
- González-Duarte A, Calleja JH, Mitre VG, et al. Simultaneous central nervous system complications of C. neoformans infection. Neurol. Int 1(1), e22 (2009).
- Lan SH, Chang WN, Lu CH, et al. Cerebral infarction in chronic meningitis: a comparison of tuberculous meningitis and cryptococcal meningitis. QJM 94(5), 247-253 (2001).
- Ecevit IZ, Clancy CJ, Schmalfuss IM, et al. The poor prognosis of central nervous system cryptococcosis among nonimmunosuppressed patients: a call for better disease recognition and evaluation of adjuncts to antifungal therapy. Clin. Infect. Dis 42(10), 1443-1447 (2006).