Research Article - Neuropsychiatry (2017) Volume 7, Issue 4
A Randomized Controlled Trial on Clinical Efficacy of Massage Therapy in a Multisensory Environment for Residents with Severe and Profound Intellectual Disabilities
- *Corresponding Author:
- Wai Tong Chien, PhD, MPhil, BN (Hons), RMN, FHKAN
Professor and Associate Head (Research)
School of Nursing
Faculty of Health and Social Sciences
The Hong Kong Polytechnic University
Hung Hom, Kowloon, Hong Kong SAR, China
Tel: (852) 2766 5648
Fax: (852) 2364 9663
Abstract
Abstract
Institutional care is the major service provision for persons with severe and profound intellectual disabilities because of their high dependence on daily living activities and physical illness. The daily schedule is usually non-stimulating and monotonous, which can be the contributing factors of their challenging behaviours. Recent literature has suggested that relaxation activities could reduce their challenging behaviours due to the counteractive effect of muscle relaxation on psychological distress. Despite having inconclusive evidence, multisensory environment and massage therapy have been increasingly used to manage challenging behaviours.
Methods
A clinical trial was conducted in a long-term care facility in Hong Kong to evaluate the effects of multisensory environment, massage therapy and their combined use on reducing the challenging behaviours and improving positive behaviours of residents with severe and profound intellectual disabilities. All eligible residents were recruited and then randomly assigned to wither one of three treatment groups, or usual care only (n=31-34/group) for 10- week intervention after a one-month washout period. Outcome measures, including a few behavioural measures and physiological data, were assessed at recruitment and immediately and 2 weeks after completed the 10-week intervention.
Results
A total of 129 participants (63 male and 66 female) completed the study. There were significant improvements in respiration rate, adaptive behaviours and sleepy state in all study groups. Participants in massage therapy had significantly greater increases in their number and duration of adaptive behaviours over 2-week follow-up than those in usual care; and they also showed greater reduction in sleepiness during and after the intervention.
Conclusion
Short-lived positive effect of massage therapy and/or multisensory environment on challenging behaviours was found during and immediately after interventions. However, this positive effect could not be sustained when observed in the residential unit over the 2-week follow-up. Hence, there is a need for additional intervention strategies in promoting these residents’ positive and adaptive behaviours to enhance longer-term effects of massage therapy and multisensory environment and thus reduced their challenging behaviours in the units.
Keywords
Severe and profound intellectual disability; Massage therapy; Multisensory environment; Challenging behaviours; Relaxation; Alertness
Introduction
The prevalence of persons with severe and profound intellectual disabilities (SPID) comprises about 5% among intellectual disability population [1]. The service provisions for this group of people are predominant on residential care because of their severe cognitive impairments and marked and profound physical disabilities [2]; in which the most fragile and vulnerable SPID persons are eligible in long-term institutional care where the daily schedule is usually highly structured and the environment is monotonous. This could be a contributing factor to the occurrence of challenging behaviours [3]. In fact, a survey has shown that more difficult challenging behaviours such as self-injurious behaviours were often exhibited in people with severe to profound intellectual disabilities [4]. The high incidence of challenging behaviours definitely increases the cost of service provision in current restrictive treatment and management practices on manpower, chemical and mechanical sedations and enhancement of structuring or organisation of their living environment [5]. The exhibition of challenging behaviours not only affects the social orders of the environment but also possibly harm to others and oneself. More importantly, these kinds of behaviours can limit the persons from access to community facility and social integration, thus jeopardizing one’s quality of life [6].
Recent literature has suggested that relaxation activities can reduce the challenging behaviours because muscle relaxation is counteractive to emotional arousal and psychological distress [3]. The incidence of sensory damage is common among persons with SPID, the more severe of the disability, the more the sensory deficits, especially cerebral visual impairment [7]. To compensate visual and hearing deficits, massage therapy is adopted to fulfill the basic desire for sensory pleasure.
The use of hand massage is believed to promote relaxation and body awareness of persons with SPID. The relationship between residents and staff can be substantially improved due to physical proximity and tenderness during the massage process [8]. Recent literature also suggest that positive behaviours such as increased attention to immediate environment, eye contacts and initiatives in social interactions can be increased after MSE sessions [3,9].
Studies using single mode/modality of intervention (massage therapy or MSE) showed modest effects in muscle relaxation and anxiety reduction [8,9], as well as increase of positive behaviours [3,9]. However, there are not any study to test a combined mode of these modalities [massage therapy (MT) plus MSE; MT-MSE], which might have echoed or accentuated effects to the participants. Most positive assertions of using massage therapy and MSE were come from personal clinical experiences, not properly evaluated by scientific study. Yet a few studies reported no significant relaxation outcome after MSE and massage therapy [10,11], several recent research reported MSE could exert significant effect on reducing challenging behaviours [10,11]. These inconsistent findings make us difficult to draw a conclusion on the effects of MSE and/or massage therapy. Therefore, the aim of this study was to evaluate and compare the clinical effectiveness of MT, MSE and their combined use (MT-MSE) for residents with severe and profound intellectual disabilities on reducing their challenging behaviours and other physiological and psychosocial outcomes such as alertness and heart and respiration rates (indicating level of anxiety).
The primary outcome was the frequency and severity of challenging behaviours in usual care environment measured with Behaviour Problems Inventory (BPI-01). The secondary outcomes were heart and respiration rates (physiological state), alertness level using Alertness Observation Checklist (AOC), and maladaptive and adaptive behaviours using Behaviour Checklist (BC).
The objectives of the study were:
• To compare treatment effects between the three alternative treatment groups (MSE, MT and MT-MSE) and usual care (control group) for participatns with SPID on improving challenging behaviours (primary outcome) and secondary outcomes at immediately after completion of the 10- week intervention; and
• To examine the comparative carryover effects of the three interventions between study groups at a two-week follow-up.
The study hypotheses included that when compared with the usual care group, there were:
1. Significantly greater reductions of frequency and severity of challenging behaviours of the participants in the three intervention groups after completed the interventions.
2. Significantly more improvements in the following secondary outcomes of the participants in the treatment groups immediately after the interventions:
a. Stable and normal heart and respiration rates (i.e., low bodily excitement and less anxiety);
b. Alertness state showing awareness to the immediate environment and maintaining social contacts; and
c. Reduced maladaptive behaviours and increased adaptive behaviours.
3. Significantly larger carryover effects at 2-week follow-up on the primary and secondary outcomes in the three treatment groups.
In addition, the fourth study hypothesis was:
4. The participants in the combined MT-MSE intervention would indicate a significantly greater reduction in maladaptive behaviours and increase of alertness state than the other two interventions (MT only and/or MSE only).
Materials and Methods
▪ Research setting
The study venue was the largest 500-bed specialized institution for adults with SPID in Hong Kong that provided comprehensive infirmary and rehabilitation care in 10 residential units. The institution was governed by Hospital Authority (HA), Hong Kong. Apart from severe and profound intellectual disabilities, most of the residents also suffered from physical or multiple types of disabilities.
▪ Subjects
Since the study objectives and outcomes focused on frequency and severity of challenging behaviours, only those residents who exhibited at least one type of challenging behaviours over the past two months were recruited. Their eligibility to participate the study was based on the inclusion and exclusion criteria as stipulated at below.
▪ Inclusion and exclusion criteria
The inclusion criteria of the participants included:
• admitted for at least 3 months to provide sufficient time for the formal carers to get familiar with their usual behaviour patterns and avoid misinterpretations of their bizarre behaviours; for instance, some residents might show restlessness and irritability when suffering from constipation or starting to adapt a new residential environment;
• aged 18 to 64 years adults who might have comparable mechanoreceptors’ sensitivity to external pressure, which declined along with age, especially in the nerve endings over palms [12,13].
• Those with the following conditions were excluded from the study:
• seriously ill or complete bed-rest residents who were not allowed to join outside ward activities or transferring out of bed due to physical fragility;
• having infectious diseases e.g., Methicillinresistant staphylococcus aureus (MRSA) to prevent cross infection;
• frequently discharged to general hospital or having frequent home leave which would interrupt the intervention and assessment process;
• being restless and resistive to stay in MSE;
• having instruction from case medical doctor to suspend massage therapy; and
• having severe contracture and deformities of both hands and feet, which could affect the use/effect of massage therapy.
Due to limited studies in this topic, the estimated sample size was calculated based on Cohen’s conventional effect size estimation in social and behavioural research [14]. With repeated-measures ANOVA tests used for within and between group comparisons, it was estimated 45 participants in each study group to achieve a medium Cohen’s effect size (f=0.25) at significance level of 0.05 and study power of 0.8. Considering 10% of potential attrition rate [3,9], 46 participants in each group were randomly recruited to meet the minimum sample size required (i.e., a total of 184 residents with SPID to be recruited). However, only 186 out of 493 residents in the 10 units under study met the inclusion and exclusion criteria, thus being slightly below the planned sample size (186 participants) and all of the eligible participants were recruited in this study. The relatives or guardians of all these 186 eligible residents were invited to give proxy consent and finally, 131 proxy consents obtained to agree on their residents to participate the study.
The whole study period was 12 weeks, in which duration of interventions were 10 weeks. The outcome measures were taken at recruitment before the allocation of group assignment, (T0), midway progress checking at week 5 (T1), immediately after completed the interventions at week 10 (T2), and 2-week follow-up at week 12 (T3). There was no intervention given between week 10 and week 12 in order to investigate any carry-over effects of any of the three modalities of interventions used.
Since the study population might receive massage therapy and MSE before the study, the participants were required to undergo one-month washout period to avoid contamination effects of the intervention tested in the study. The recommended one-month washout period and two-week follow-up study were based on the findings of previous literature [15-17], in which the results revealed non-significant carryover effect 1-3 weeks following the MT or MSE interventions.
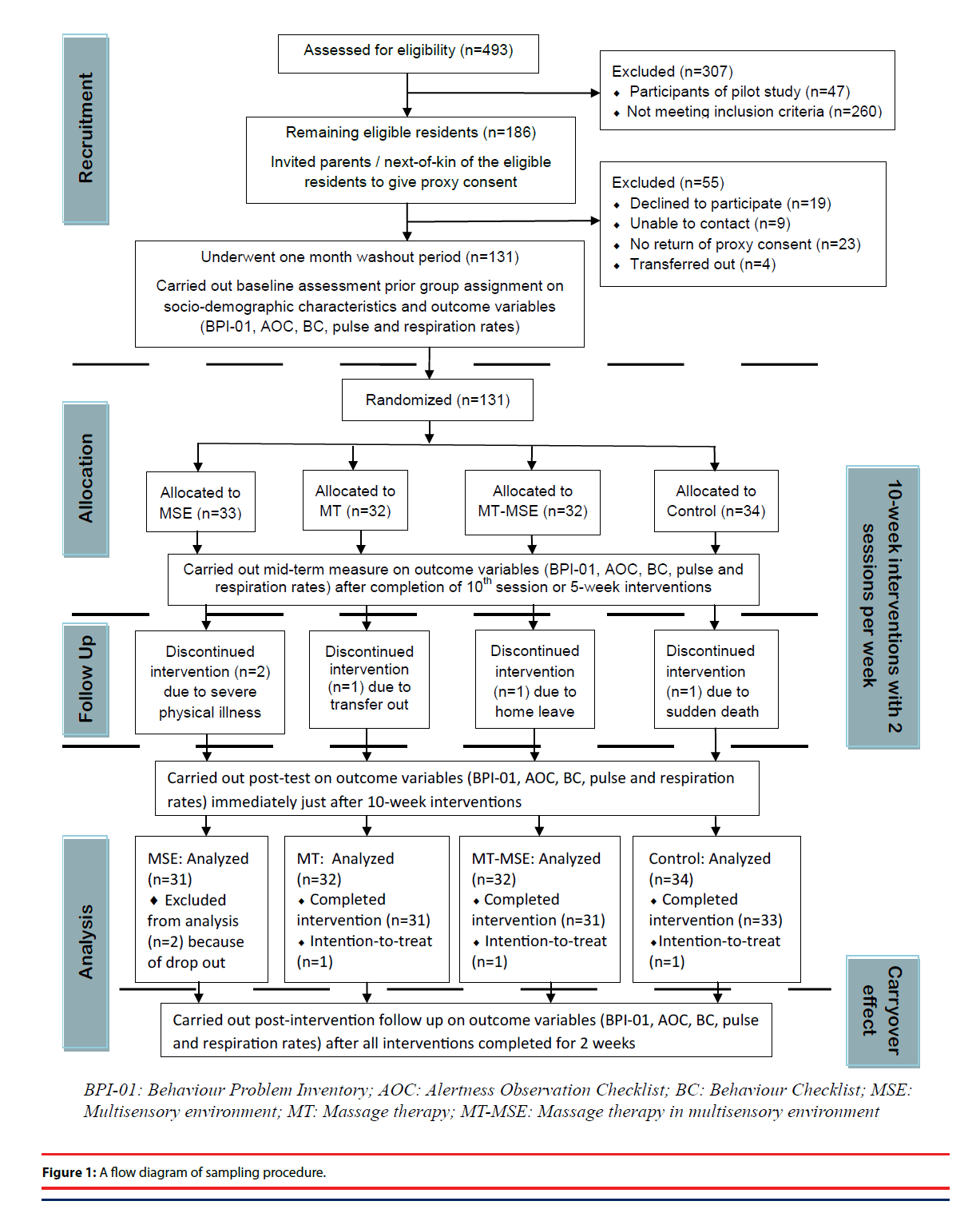
After the washout period, all of them completed the baseline measurement on their demographic and clinical characteristics and study outcomes. A clinical staff, who was blind and concealed to the participant list in each unit, was invited to draw one card with 4 numbers in random orders (e.g., 1234, 3241 or 2341; whereas, 1=MSE alone, 2=MT alone, 3=MT-MSE, and 4=usual care) in blocks. The number of draws was depended on number of participants in the units, so that participants were randomly and evenly assigned into each of the four study groups. Just beginning of the interventions, two MSE participants dropped out because of severe physical illness. The remaining 129 participants continued the study, and finally 126 participants completed all assessments from T1 to T3. Three participants could not be contacted/followed-up over the study period, in which two participants discontinued the interventions after midway checking of the intervention progress (T1) because one was transferred out to another clinical unit and another one died suddenly. The third drop-out participant completed the interventions and the first post-test (T2) immediately after intervention, and then had a long period of home leave and thus was unable to complete the second post-test (T3). In order to increase statistical power, intentionto- treat principle [18] was applied with using last observation carried forward method for imputation the missing data of the three participants. Finally, data of 129 participants were analyzed with 126 full data set and three partially completed data, the overall attrition rate was 3.8%. Details of the sampling and study procedures according to the latest CONSORT statement [19] are presented in Figure 1.
▪ Interventions
Multisensory environment (MSE)
Based on the design of 20 MSE studies [3,20], the most common MSE intervention protocol for people with ID was 30 minutes twice per week for 20 sessions (consecutive 10 weeks). Hence, this study adopted the same MSE protocol for the participants. During their stay in the MSE, the residents were accompanied by a care staff who acted as an enabler to facilitate the interaction with different kinds of sensory equipment based on individual needs and/or preferences. All participants were encouraged to choose their preferred equipment to meet the basic principle of entertaining their free choices in the MSE. In reality, many of the participants were unable to indicate explicitly their preference; thus, choices were made by the staff. Their facial expression was often the best indicator to show their acceptance to the designated equipment.
Since the use of MSE as leisure activity was common in research setting, the preparation of the MSE session has already been established prior the study. Hence, check of treatment integrity was not scheduled in regular basis by the researchers.
Massage therapy (MT)
The time schedule of massage therapy that adopted in this study was synthesized from two meta-analyses of 56 articles [17,21], in terms of minutes per session, number of sessions for each participant, and length of intervention period.
Participants of the MT group received 15-minute either hand or foot massage twice per week for a consecutive 10-week period. Three designated nursing staff were trained to perform the massage therapy. The massage protocol was adopted from a massage guideline for people with ID [22]. Face validity of the massage protocol was confirmed by two training organizations. Regular monitoring based on protocol checklist was scheduled to ensure treatment fidelity and integrity, especially in the first several sessions by a researcher who was a qualified massage therapist. Benchmark with 90% accuracy to the checklist implied good compliance. ‘Surprise’ checks were also conducted to control deviation from the massage protocol.
Massage therapy in multisensory environment (MT-MSE)
Participants of the MT-MSE group received both 30-minute MSE and 15-minute massage therapy twice a week for consecutive 10 weeks. During the 30-minute stay in MSE, a 15-minute MT was applied in the first 15-minute and then the participant focused in the activities in the MSE in the last 15 minutes. An enabler accompanied the participant throughout the session. Schedule of treatment fidelity and integrity check was the same as MT.
Control group
Participants in the control group stayed in their usual care environment and followed their daily schedule as usual without the involvement of MT and MSE activities throughout the study period over the 10-week intervention. Residents mostly spent their free times in watching television or listening to music. To balance the enabler’s effect between the other study groups, attention and social interaction with a frontline staff were arranged individually twice a week with 15 minutes per session. The researchers carried out irregular inspection to monitor the progress throughout the study period. After the 10-week intervention, all participants of the four study groups received the routine care from weeks 11 to 12 (as follow-up).
▪ Instruments
Behaviour Problems Inventory (BPI-01)
The BPI-01 was especially designed for studying on the prevalence of behavioural problems of people with ID, as well as for repeated measurements of treatment outcome in terms of those observed problem behaviours in the scale [23]. BPI-01 consisted of 49 items with three subscales and been widely employed in people with profound ID who lived in residential setting. This instrument was to evaluate the frequency and severity of challenging behaviours that exist for the previous two months. In order to unify the assessment period in the study, the assessors were required to rate the behaviours that existed in the usual care for previous two weeks.
Alertness Observation Checklist (AOC)
The AOC [24] was especially designed to detect the optimal alertness state or the “right moment” for interaction and learning where resident’s attention to the immediate environment was strong. The AOC was an interval scoring checklist. It was used to identify the influence of various stimuli on alertness, including visual, tactile and auditory, in order to assess the effect of the interventions on the participant’s alertness level. A 20-second observation interval was adopted during the intervention period as suggested by the original authors of AOC. AOC contained five levels of alertness states where the active state of green color separated into two categories: one was active alert state (G1) where body movement was exhibited, and passive alert state (G2) where no body movement was noted but the person was still in contact with the immediate environment [25]. Other levels of alertness included amber for inactivity and withdrawal, red for sleepy or drowsy state, and blue for agitation and discontentment.
Behaviour Checklist (BC)
The behaviour checklist (BC) was developed by Shapiro et al. [26] to assess the behavioural reactions toward MSE and relevant psychological intervention, e.g., social interactions. The Checklist consisted of 22 items in which 16 items were for self-stimulating behaviours (SSB) and 6 items for adaptive behaviours (AB). The observations of SSB and AB were based on 1-minute interval to assess the number of exhibited behaviours during the intervention. In order to avoid term confusion on stereotypic behaviour of the BPI-01, the SSB of BC was renamed as maladaptive behaviours (MB) in the study.
Data processing
All quantitative data collected were analyzed using the statistical software IBM SPSS for Windows, version 21. Descriptive statistics were used to summarize the socio-demographic and clinical data such as age, gender, mobility level, and feeding mode. The normality of the measure outcomes was checked and revealed that all continuous data did not fulfill the normal distribution. Hence, nonparametric test was used to analyze the baseline data of the outcome measures to identify any differences between study groups, then Generalized Estimating Equations (GEE) tests, which could be used for both categorical and continuous data [27] irrespective to sample size, was applied to identify the interaction effects (i.e., time and group effects) between groups, and time effects within groups. When significant differences found between groups, contrast comparisons were automatically carried out in the GEE test. The level of significance of all statistical tests was set at 0.05 with two-tailed.
Ethical considerations
The research protocol was approved by the Human Subjects Research Ethics Committee of The Hong Kong Polytechnic University and the Cluster Clinical Research Ethics Committee of Hong Kong Hospital Authority. The study was also registered in “ClinicalTrial.gov” with registration number (identifier): NCT02120820.
The written information sheet which stated the purpose of the study and the proxy consent form were given to the participants’ guardians and parents. They were reassured that they could refuse to participate in the study or withdraw from the study at any time, and such refusal or withdrawal would not affect the treatment plan of the residents with SPID. Anonymity and confidentiality of the participants’ data were strictly assured and personal identity of individual participants was not disclosed.
The interventions basically caused no harm to the participants, even if no significant benefits identified. The instruments selected and employed were non-invasive and harmless to the study participants. If the challenging behaviours, especially those self-harm and violence increased dramatically during the study process, urgent medical consultation would be made by the researcher / primary nurse. In fact, none of the participants showed discontentment and restlessness, and there were not any adverse events reported throughout the study period.
Results
▪ Ethical considerations
The final sample (n=129) comprised 63 male (48.8%) and 66 female (51.2%), with a mean age of 47 years (SD=10.93; range 18-64 years). In view of comorbidities, around 66% suffered from epilepsy, 93% of them were taking regular medications, in which, 76% involved antiepileptic and psychotropic drugs. More than half (51.2%) of the participants was required adaptive support, including body alignment support, safety belt and limb holders in daily care. More than 70% of them required staff assistance in continence care, feeding, and physically transfer; whereas, all required assisted and/or trolley bathing. About 22% and 31% of them had hearing and visual impairments respectively. The demographic and clinical characteristics of the participants are summarized in Table 1. These demographic and clinical characteristics showed no statistical differences between the four study groups (using Chi-square test, p=0.07-0.98).
| Characteristics | Total (n=129) | MSE (n=31) | MT (n=32) | MT-MSE (n=32) | Control (n=34) | Pearson Chi square c2 | p- value |
|---|---|---|---|---|---|---|---|
| Mean age# (SD) | 47 (10.93) | 45.29 (10.52) | 48.22 (11.77) | 46.22 (11.25) | 48.12 (10.39) | 0.552 | 0.648 |
| Gender | 0.205 | 0.977 | |||||
| Male | 63 (48.8%) | 16 (51.6%) | 16 (50%) | 15 (46.9%) | 16 (47.1%) | ||
| Female | 66 (51.2%) | 15 (48.4%) | 16 (50%) | 17 (53.1%) | 18 (52.9%) | ||
| Adaptive support | 3.047 | 0.384 | |||||
| Yes | 66 (51.2%) | 18 (58.1%) | 15 (46.9%) | 13 (40.6%) | 20 (58.8%) | ||
| No | 63 (48.8%) | 13 (41.9%) | 17 (53.1%) | 19 (59.4%) | 14 (41.2%) | ||
| Bathing mode | 1.389 | 0.708 | |||||
| Assisted | 20 (15.5%) | 4 (12.9%) | 7 (21.9%) | 4 (12.5%) | 5 (14.7%) | ||
| Trolley | 109 (84.5%) | 27 (87.1%) | 25 (78.1%) | 28 (87.5%) | 29 (85.3%) | ||
| Cerebral palsy | 3.188 | 0.364 | |||||
| Yes | 30 (23.3%) | 7 (22.6%) | 6 (18.8%) | 11 (34.4%) | 6 (17.6%) | ||
| No | 99 (76.7%) | 24 (77.4%) | 26 (81.3%) | 21 (65.6%) | 28 (82.4%) | ||
| Continence level | 3.618 | 0.306 | |||||
| Yes | 33 (25.6%) | 8 (25.8%) | 12 (37.5%) | 6 (18.8%) | 7 (20.6%) | ||
| No | 96 (74.4%) | 23 (74.2%) | 20 (62.5%) | 26 (81.3%) | 27 (79.4%) | ||
| Epilepsy | 2.494 | 0.476 | |||||
| Yes | 85 (65.9%) | 23 (74.2%) | 19 (59.4%) | 19 (59.4%) | 24 (70.6%) | ||
| No | 44 (34.1%) | 8 (25.8%) | 13 (40.6%) | 13 (40.6%) | 10 (29.4%) | ||
| Feeding mode | 4.596 | 0.868 | |||||
| Independent | 38 (29.5%) | 7 (22.6%) | 13 (40.6%) | 8 (25%) | 10 (29.4%) | ||
| Assisted | 24 (18.6%) | 7 (22.6%) | 5 (15.6%) | 6 (18.8%) | 6 (17.6%) | ||
| Dependent | 55 (42.6%) | 14 (45.2%) | 10 (31.3%) | 15 (46.9%) | 16 (47.1%) | ||
| Enteral | 12 (9.3%) | 3 (9.7%) | 4 (12.5%) | 3 (9.4%) | 2 (5.9%) | ||
| Hearing loss | 2.091 | 0.554 | |||||
| Yes | 29 (22.5%) | 6 (19.4%) | 8 (25%) | 5 (15.6%) | 10 (29.4%) | ||
| No | 100 (77.5%) | 25 (80.6%) | 24 (75%) | 27 (84.4%) | 24 (70.6%) | ||
| Medication | 6.485 | 0.090 | |||||
| Yes | 120 (93%) | 30 (96.8%) | 29 (90.6%) | 32 (100%) | 29 (85.3%) | ||
| No | 9 (7.0%) | 1 (3.2%) | 3 (9.4%) | 0 | 5 (14.7%) | ||
| Antiepileptic and psychotropic drugs | 7.153 | 0.067 | |||||
| Yes | 98 (76%) | 28 (90.3%) | 21 (65.6%) | 26 (81.3%) | 23 (67.6%) | ||
| No | 31 (24%) | 3 (9.7%) | 11 (34.4%) | 6 (18.8%) | 11 (32.4%) | ||
| Mobility level | 1.733 | 0.943 | |||||
| Ambulant | 32 (24.8%) | 7 (22.6%) | 10 (31.3%) | 6 (18.8%) | 9 (26.5%) | ||
| Chair-bound | 71 (55%) | 17 (54.8%) | 17 (53.1%) | 19 (59.4%) | 18 (52.9%) | ||
| Bedridden | 26 (20.2%) | 7 (22.6%) | 5 (15.6%) | 7 (21.9%) | 7 (20.6%) | ||
| Traceable relative | 4.306 | 0.230 | |||||
| Yes | 100 (77.5%) | 27 (87.1%) | 21 (65.6%) | 25 (78.1%) | 27 (79.4%) | ||
| No | 29 (22.5%) | 4 (12.9%) | 11 (34.4%) | 7 (21.9%) | 7 (20.6%) | ||
| Visual impairment | 2.919 | 0.404 | |||||
| Yes | 40 (31%) | 12 (38.7%) | 8 (25%) | 12 (37.5%) | 8 (23.5%) | ||
| No | 89 (69%) | 19 (61.3%) | 24 (75%) | 20 (62.5%) | 26 (76.5%) |
SD=Standard deviation; MSE=Multisensory Environment, MT=Massage Therapy, MT-MSE=Massage Therapy in Multisensory Environment
Table 1: Demographic and clinical characteristics of participants among four groups (n=129).
▪ Outcome measures at baseline
The results of the baseline outcome assessment are summarized in Table 2. There were no significant differences on all of the outcome scores at baseline between the four study groups (p=0.108-1.000). The mean scores of the subscales [self-injurious behaviours (SIB), self-stereotyped behaviours (SSB) and aggressive behaviours] of challenging behaviours (primary outcome) also showed nonsignificant differences. There was a wide range of self-stereotypic behaviours exhibited among the participants, while aggressive behaviour was the least (seldom) displayed one that may be caused by the physical disablement or use of adaptive support to restrict body movement.
| Variables | MSE (n=31) | MT (n=32) | MT-MSE (n=32) | Control (n=34) | Kruskal Wallis H test (df=3) | p value |
|---|---|---|---|---|---|---|
| Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) | |||
| Primary Outcome | Behaviour Problem Inventory (BPI-01) | |||||
| CB_frequency scale | 9.66 (2.45) | 11.05 (2.41) | 8.80 (2.41) | 7.47 (2.34) | 1.77 | 0.622 |
| CB_severity scale | 5.08 (1.89) | 5.24 (1.86) | 4.63 (1.86) | 3.94 (1.81) | 1.57 | 0.666 |
| SIB_frequency scale | 3.32 (0.65) | 2.71 (0.64) | 3.10 (0.64) | 2.30 (0.62) | 0.92 | 0.821 |
| SIB_severity scale | 1.90 (0.45) | 1.49 (0.44) | 1.80 (0.44) | 1.37 (0.43) | 0.64 | 0.888 |
| SSB_frequency scale | 5.81 (1.49) | 7.12 (1.46) | 4.62 (1.46) | 4.66 (1.42) | 1.48 | 0.686 |
| SSB_severity scale | 2.82 (1.05) | 3.15 (1.03) | 2.20 (1.03) | 2.23 (1.00) | 2.31 | 0.512 |
| Aggression_frequency scale | 0.59 (0.56) | 1.24 (0.56) | 1.15 (0.56) | 0.57 (0.54) | 1.13 | 0.769 |
| Aggression_severity scale | 0.40 (0.47) | 0.63 (0.46) | 0.68 (0.46) | 0.40 (0.45) | 0.92 | 0.821 |
| Secondary Outcomes | ||||||
| Pulse / minute | 83.66 (2.71) | 83.43 (2.67) | 84.13 (2.67) | 81.10 (2.59) | 0.23 | 0.973 |
| Respiration / minute | 17.46 (0.56) | 19.59 (0.55) | 18.19 (0.55) | 18.00 (0.53) | 6.07 | 0.108 |
| Behaviour Checklist (BC) | ||||||
| No. of MB/minute | 4.42 (1.21) | 4.71 (1.19) | 2.25 (1.19) | 4.89 (1.16) | 2.84 | 0.416 |
| No. of AB/minute | 0.09 (1.18) | 0.81 (1.16) | 0.78 (1.16) | 0.16 (1.12) | 2.10 | 0.553 |
| Duration of MB (minute) | 3.30 (0.10) | 4.04 (0.89) | 2.20 (0.89) | 4.37 (0.86) | 2.67 | 0.446 |
| Duration of AB (minute) | 0.09 (0.75) | 0.80 (0.74) | 0.74 (0.74) | 0.17 (0.71) | 2.10 | 0.553 |
| Alertness Observation Checklist (AOC)@ | ||||||
| Green 1: active alert | 5.31% (0.05) | 4.65% (0.05) | 3.75% (0.04) | 4.97% (0.05) | 1. 10 | 0.799 |
| Green 2: passive alert | 1.65% (0.02) | 7.99% (0.08) | 4.93% (0.05) | 3.99% (0.04) | 0.99 | 0.803 |
| Amber: inactive | 38.56% (0.39) | 66.53% (0.67) | 48.4% (0.48) | 60.39% (0.60) | 3.11 | 0.375 |
| Red: sleepy | 54.48% (0.54) | 20.83% (0.21) | 42.92% (0.43) | 30.65% (0.31) | 4.55 | 0.207 |
| Blue: discontented | 0 | 0 | 0 | 0 | 0 | 1.000 |
@ Percentage of occurrence of individual alertness levels (conversion of percentage into decimal figure) MSE=Multisensory Environment, MT=Massage Therapy, MT-MSE=Massage Therapy in Multisensory Environment, SE=Standard Error, CB=Challenging Behaviour, SIB=Self-injurious Behaviour, SSB=Self-stereotypic Behaviour, MB=Maladaptive Behaviour, AB=Adaptive Behaviour
Table 2: Baseline assessment of different outcome measures among four study groups.
Regarding the secondary outcomes, there was no significant difference on the physiologic signs of pulse and respiration rates among the four groups. From the mean values of maladaptive (M=2.20-4.89) and adaptive (M=0.09-0.81) behaviours, the participants appeared to be more often engaged with maladaptive behaviours at baseline measurement.
According to the percentages of different types of alertness, inactive with withdrawn (ranged from 39-67%) and sleepy (ranged from 21- 54%) behaviours were the most common ones among the four study groups. Indeed, none of the participants showed discontentment and restlessness.
▪ Interim progress of the outcome measures
The purpose of interim measure was to check the intervention progress of the participants at the end of week 5 during the 10-week interventions. Only secondary outcomes showed significant interaction effects (group x time) on respiration rates and passive alertness state. In which, the MT-MSE participants showed the lowest respiration rates and highest passive alertness state than other study groups. The results of primary outcome (frequency and severity of challenging behaviours) showed no significant difference between groups.
It is important to note that throughout the study period, there were no discontented or restless behaviours observed among the four groups and thus this discontented state (blue color) was excluded from the final outcome analysis.
▪ Overall treatment effects
The mean scores and standard errors of the outcome measures from the baseline (T0) to 2-week post-intervention (carryover effect at T3) are shown in Table 3. The overall interaction effects (time x group) were identified in respiration rate [Wald χ2 (6) =37.46, p=0.0001], number of maladaptive behaviour [Wald χ2 (6) =14.03, p=0.029], number of adaptive behaviour [Wald χ2 (6) =20.37, p=0.002], and duration of adaptive behaviour [Wald χ2 (6) =20.87, p=0.002]. Among the four outcome measures, only respiration rate and duration of adaptive behaviour also revealed statistical different in group effect and time effect.
| MSE (n=31) | MT (n=32) | MT-MSE (n=32) | Control (n=34) | GEE (Time) | GEE (Group) | GEE (Time*Group) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T0 Mean (SE) | T2 Mean (SE) | T3 Mean (SE) | T0 Mean (SE) | T2 Mean (SE) | T3 Mean (SE) | T0 Mean (SE) | T2 Mean (SE) | T3 Mean (SE) | T0 Mean (SE) | T2 Mean (SE) | T3 Mean (SE) | Wald χ2 (df=2) | p value | Wald χ2 (df=3) | p value | Wald χ2 (df=6) | p value | |
| Primary Outcome | ||||||||||||||||||
| Frequency of CB | 9.81 (2.07) | 7.45 (1.75) | 7.23 (1.79) | 11.16 (2.15) | 7.63 (1.56) | 7.03 (1.39) | 9.00 (2.16) | 6.47 (1.45) | 6.50 (1.65) | 7.62 (1.04) | 7.06 (1.31) | 5.62 (1.16) | 40.73 | 0.000 *** | 1.03 | 0.794 | 10.67 | 0.099 |
| Severity of CB | 5.19 (1.23) | 4.23 (1.15) | 4.06 (1.19) | 5.41 (1.22) | 4.53 (1.28) | 4.09 (1.11) | 4.84 (1.48) | 3.84 (1.12) | 3.84 (1.22) | 4.06 (0.59) | 3.76 (0.79) | 2.94 (0.60) | 40.91 | 0.000 *** | 0.94 | 0.816 | 5.90 | 0.434 |
| Secondary Outcomes | ||||||||||||||||||
| Pulse rate | 83.52 (2.69) | 79.00 (2.33) | 78.39 (2.14) | 83.47 (2.63) | 79.91 (2.42) | 79.59 (1.95) | 83.88 (2.61) | 79.78 (2.77) | 80.97 (2.50) | 80.91 (1.82) | 84.71 (2.73) | 85.29 (3.59) | 3.43 | 0.180 | 1.57 | 0.667 | 9.03 | 0.172 |
| Respiration rate | 17.45 (0.52) | 16.16 (0.49) | 15.77 (0.38) | 19.59 (0.64) | 17.16 (0.47) | 16.53 (0.41) | 18.19 (0.55) | 15.72 (0.41) | 15.91 (0.30) | 18.00 (0.53) | 19.38 (0.72) | 19.35 (0.58) | 27.57 | 0.000 *** | 25.02 | 0.000 *** | 37.46 | 0.000 *** |
| Behaviour Checklist | ||||||||||||||||||
| No. of maladaptive behaviour | 4.45 (1.42) | 3.63 (1.19) | 4.13 (1.00) | 4.75 (1.30) | 2.19 (0.55) | 5.41 (1.28) | 2.28 (0.81) | 4.97 (1.28) | 4.47 (0.97) | 4.91 (1.20) | 4.85 (1.55) | 2.91 (0.89) | 0.30 | 0.862 | 0.09 | 0.993 | 14.03 | 0.029* |
| No. of adaptive behaviour | 0.10 (0.05) | 6.77 (1.24) | 0.94 (0.37) | 0.88 (0.48) | 8.09 (1.90) | 6.50 (1.58) | 0.69 (0.50) | 4.19 (1.17) | 1.25 (0.50) | 0.21 (0.12) | 4.85 (1.08) | 4.44 (1.24) | 81.94 | 0.000 *** | 7.35 | 0.062 | 20.37 | 0.002 ** |
| Duration maladaptive behaviour | 3.32 (0.88) | 2.90 (0.79) | 3.58 (0.80) | 4.06 (1.00) | 2.19 (0.55) | 4.69 (0.95) | 2.22 (0.77) | 4.06 (0.90) | 4.41 (0.96) | 4.38 (1.00) | 3.68 (0.88) | 2.76 (0.82) | 1.98 | 0.371 | 0.23 | 0.973 | 10.35 | 0.111 |
| Duration adaptive behaviour | 0.10 (0.05) | 5.27 (0.87) | 0.84 (0.33) | 0.84 (0.46) | 5.38 (0.94) | 4.72 (0.91) | 0.66 (0.47) | 3.38 (0.84) | 1.22 (0.48) | 0.21 (0.12) | 4.56 (1.00) | 3.59 (0.81) | 98.02 | 0.000 *** | 9.34 | 0.025* | 20.87 | 0.002 ** |
| Alertness Observation Checklist@ | ||||||||||||||||||
| Green 1_Active alert | 5.31% (0.05) | 36.24% (0.36) | 21.72% (0.22) | 4.65% (0.05) | 38.13% (0.38) | 30.35% (0.30) | 3.75% (0.04) | 29.38% (0.29) | 24.44% (0.24) | 4.97% (0.05) | 32.54% (0.33) | 24.51% (0.25) | 83.12 | 0.000 *** | 0.66 | 0.883 | 1.66 | 0.948 |
| 2.39 (1.35) | 16.31 (2.71) | 9.77 (2.81) | 2.09 (1.17) | 17.16 (3.51) | 13.66 (3.28) | 1.69 (1.39) | 13.22 (2.91) | 11.00 (2.63) | 2.24 (1.56) | 14.65 (3.08) | 11.03 (2.82) | |||||||
| Green 2_Passive alert | 1.65% (0.02) | 42.76% (0.43) | 25.3% (0.25) | 7.99% (0.08) | 46.66% (0.47) | 38.96% (0.39) | 4.93% (0.05) | 58.54% (0.59) | 20.9% (0.21) | 3.99% (0.04) | 38.5% (0.39) | 35.69% (0.36) | 159.69 | 0.000 *** | 2.90 | 0.407 | 9.13 | 0.167 |
| 0.74 (0.31) | 19.24 (2.56) | 11.39 (2.87) | 3.59 (1.66) | 20.38 (3.19) | 17.53 (3.27) | 2.22 (1.40) | 26.34 (2.98) | 9.41 (2.61) | 1.79 (0.85) | 17.32 (2.96) | 16.06 (3.09) | |||||||
| Amber_Inactive level | 38.56% (0.39) | 15.66% (0.16) | 26.67% (0.27) | 66.53% (0.67) | 11.6% (0.12) | 24.93% (0.25) | 48.4% (0.48) | 5.9% (0.06) | 36.53% (0.37) | 60.39% (0.60) | 20.72% (0.21) | 26.08% (0.26) | 94.21 | 0.000 *** | 1.13 | 0.770 | 8.32 | 0.216 |
| 24.52 (3.61) | 7.05 (2.51) | 12.00 (3.05) | 29.94 (3.19) | 5.22 (1.81) | 11.22 (2.89) | 21.78 (3.51) | 2.66 (1.47) | 16.44 (3.27) | 27.18 (3.19) | 9.32 (2.46) | 11.74 (2.99) | |||||||
| Red_Sleepy level | 54.48% (0.54) | 5.34% (0.05) | 26.31% (0.26) | 20.83% (0.21) | 3.61% (0.04) | 5.76% (0.06) | 42.92% (0.43) | 6.18% (0.06) | 18.13% (0.18) | 30.65% (0.31) | 8.24% (0.08) | 13.72% (0.14) | 54.50 | 0.000 *** | 10.61 | 0.014* | 8.66 | 0.194 |
| 17.35 (3.68) | 2.40 (1.13) | 11.84 (3.48) | 9.38 (2.82) | 1.63 (1.16) | 2.59 (1.50) | 19.31 (3.63) | 2.78 (1.61) | 8.16 (2.33) | 13.79 (3.22) | 3.71 (1.43) | 6.18 (2.37) | |||||||
*p<0.05, **<0.01, ***<0.001 @ Percentage of occurrence of alertness level (conversion of percentage into decimal figure)
MSE=Multisensory Environment, MT=Massage Therapy, MT-MSE=Massage Therapy in Multisensory Environment, SE=Standard Error, CB=Challenging Behaviour, MD=Mean Difference, p=significance level
Table 3: Mean and standard error of primary and secondary outcome measures from baseline to carryover effect.
Significant group effect was detected in respiration rate [Wald χ2 (3)=25.02, p=0.0001], duration of adaptive behaviour [Wald χ2 (3)=9.34, p=0.025], and sleepy level of AOC [Wald χ2 (3)=10.61, p=0.014].
Time effect was prevalent among several outcome measures (i.e., p values were 0.0001), except pulse rate and number and duration of maladaptive behaviour (p=0.180-0.862). Throughout the study, the primary outcome on frequency and severity of challenging behaviour only indicated time effect [frequency: Wald χ2 (2)=40.73, p=0.0001; and severity: Wald χ2 (2)=40.91, p=0.0001].
▪ Between group effects
The contrasts tests of those significant outcome measures using their mean differences and their significance levels are presented in Table 4. The pairwise comparisons between the four study groups on the respiration rate found that all treatment groups showed significantly lower respiration rate than control group in both T2 and T3. The lowest respiration rate in T2 was in the MT-MSE and in T3, indicated in the MSE.
| Overall Treatment Effect | Respiration Rate | Number of Maladaptive Behaviour | Number of Adaptive Behaviour | Duration of Adaptive Behaviour | Sleepy Level (Red) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MD | p | ES | MD | p | ES | MD | p | ES | MD | p | ES | MD | p | ES | |
| MSE vs CTL (T2) | 3.22 | 0.000*** | 0.91 | 1.22 | 0.532 | 0.15 | 1.92 | 0.242 | 0.29 | 0.72 | 0.588 | 0.13 | 1.30 | 0.475 | 0.18 |
| MSE vs CTL (T3) | 3.58 | 0.000*** | 1.27 | 1.22 | 0.362 | 0.23 | 3.51 | 0.007** | 0.66 | 2.75 | 0.002** | 0.77 | 5.66 | 0.179 | 0.34 |
| MT vs CTL (T2) | 2.23 | 0.009** | 0.63 | 2.67 | 0.106 | 0.39 | 3.24 | 0.138 | 0.37 | 0.82 | 0.551 | 0.15 | 2.08 | 0.257 | 0.13 |
| MT vs CTL (T3) | 2.82 | 0.000*** | 0.97 | 2.49 | 0.108 | 0.40 | 2.06 | 0.306 | 0.25 | 1.13 | 0.355 | 0.23 | 3.58 | 0.201 | 0.31 |
| MT-MSE vs CTL (T2) | 3.66 | 0.000*** | 1.08 | 0.12 | 0.954 | 0.01 | 0.67 | 0.675 | 0.10 | 1.18 | 0.364 | 0.22 | 0.92 | 0.667 | 0.11 |
| MT-MSE vs CTL (T3) | 3.45 | 0.000*** | 1.28 | 1.56 | 0.235 | 0.29 | 3.19 | 0.017* | 0.58 | 2.37 | 0.012* | 0.61 | 1.98 | 0.552 | 0.15 |
| MSE vs MT (T2) | 0.99 | 0.143 | 0.37 | 1.44 | 0.273 | 0.28 | 1.32 | 0.561 | 0.15 | 0.10 | 0.937 | 0.02 | 0.78 | 0.631 | 0.12 |
| MSE vs MT (T3) | 0.76 | 0.173 | 0.34 | 1.28 | 0.431 | 0.20 | 5.56 | 0.001** | 0.86 | 3.88 | 0.000*** | 1.00 | 9.25 | 0.015* | 0.62 |
| MSE vs MT-MSE (T2) | 0.44 | 0.491 | 0.17 | 1.34 | 0.443 | 0.19 | 2.59 | 0.128 | 0.38 | 1.90 | 0.116 | 0.40 | 0.38 | 0.847 | 0.05 |
| MSE vs MT-MSE (T3) | 0.13 | 0.785 | 0.07 | 0.34 | 0.807 | 0.06 | 0.31 | 0.610 | 0.13 | 0.38 | 0.515 | 0.16 | 3.68 | 0.380 | 0.22 |
| MT vs MT-MSE (T2) | 1.44 | 0.021* | 0.58 | 2.78 | 0.046* | 0.50 | 3.91 | 0.080 | 0.44 | 2.00 | 0.113 | 0.40 | 1.16 | 0.559 | 0.15 |
| MT vs MT-MSE (T3) | 0.63 | 0.221 | 0.30 | 0.94 | 0.558 | 0.15 | 5.25 | 0.002** | 0.79 | 3.50 | 0.001** | 0.85 | 5.56 | 0.045* | 0.50 |
*p<0.05, **<0.01, ***<0.001 MSE=Multisensory Environment, MT=Massage Therapy, MT-MSE=Massage Therapy in Multisensory Environment, CB=Challenging Behaviour, MD=Mean Difference, p=significance level, ES=Effect Size
Table 4: Contrast tests of significant outcome measures on mean differences and significance levels between immediate treatment (T2) and carryover effects (T3).
Regarding the number of maladaptive behaviour, it only showed significant different between MT and MT-MSE at T2 (mean difference=2.78, p=0.046, effect size=0.50), where the MT group had the lowest mean value and the MT-MSE group reached the highest value of maladaptive behaviour at T2 time-point.
The MT group obtained the highest number and longest duration of adaptive behaviour than the other three groups at T2 and T3. Generally, the participants of MT group consistently showed more adaptive behaviours than other three study groups.
Regarding the sleepy level of AOC, the MT group showed the lowest level than the other three groups at both T2 and T3. The sleepy level of the MT group was statistically significant different from the MSE group (mean difference=9.25, p=0.015, effect size=0.62) and the MT-MSE group (mean difference=5.56, p=0.045, effect size=0.50) at T3 only. This result indicated that the participants of MT group were less sleepy during the treatment sessions, and such effect was sustained to two weeks following the intervention (T3). In contrast, the participants of MSE and MT-MSE showed sleepier than MT and control groups at T3.
According to the percentage changes in AOC across the study groups, the dominant alertness states of baseline assessment were inactive and sleepy state. Similar to the findings of the interim assessment, the dominant alertness state at post-intervention assessment (T2) switched to passive alertness (ranged from 39% - 59%), especially MT-MSE group. The alertness levels were shared between passive alertness (ranged from 25% - 39%) where MT obtained the highest percentage; and inactive state (ranged from 25% - 37%) where MT-MSE got the highest percentage at T3. Although group effect of sleepy state was found across four groups, its utmost percentage reached from 8% in T2 to 12% in T3, indicating the alertness levels of most participants remained engaging in passive alertness and inactive state but not reaching a significance level.
▪Within group effects
The time effects within-group of outcome measures with significance levels are presented in Table 5. Five outcome measures only showed statistical significant in time effect in the study. They included frequency and severity of challenging behaviour, active alertness, passive alertness and inactive state.
| Time point | MSE (n=31) | MT (n=32) | MT-MSE (n=32) | Control (n=34) | GEE (Time) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| MD | p | MD | p | MD | p | MD | p | Wald χ2 (df=2) | p valu e | ||
| Frequency of CB | T0 - T2 | 2.35 | 0.004** | 3.53 | 0.003** | 2.53 | 0.053 | 0.56 | 0.400 | 40.73 | 0.000*** |
| T0 - T3 | 2.58 | 0.003** | 4.13 | 0.000*** | 2.50 | 0.022* | 2.00 | 0.002** | |||
| T2 - T3 | 0.23 | 0.499 | 0.59 | 0.052 | 0.03 | 0.934 | 1.44 | 0.003** | 8.56 | 0.003** | |
| Severity of CB | T0 - T2 | 0.97 | 0.004** | 0.88 | 0.060 | 1.00 | 0.223 | 0.29 | 0.343 | 40.91 | 0.000*** |
| T0 – T3 | 1.13 | 0.002** | 1.31 | 0.000*** | 1.00 | 0.074 | 1.12 | 0.000*** | |||
| T2 - T3 | 0.16 | 0.462 | 0.44 | 0.219 | 0.00 | 1.000 | 0.82 | 0.014* | 5.32 | 0.021* | |
| Respiration rate | T0 - T2 | 1.29 | 0.009* | 2.44 | 0.000*** | 2.47 | 0.000*** | 1.38 | 0.102 | 27.57 | 0.000*** |
| T0 - T3 | 1.68 | 0.000*** | 3.06 | 0.000*** | 2.28 | 0.000*** | 1.35 | 0.018* | |||
| T2 - T3 | 0.39 | 0.434 | 0.63 | 0.187 | 0.19 | 0.678 | 0.03 | 0.970 | 0.57 | 0.449 | |
| Number of adaptive behaviour | T0 - T2 | 6.68 | 0.000*** | 7.22 | 0.000*** | 3.50 | 0.008** | 4.65 | 0.000*** | 81.94 | 0.000*** |
| T0 - T3 | 0.84 | 0.025* | 5.63 | 0.000*** | 0.56 | 0.441 | 4.24 | 0.001** | |||
| T2 - T3 | 5.84 | 0.000*** | 1.59 | 0.342 | 2.94 | 0.012* | 0.41 | 0.795 | 14.03 | 0.000*** | |
| Duration of adaptive behaviour | T0 - T2 | 5.18 | 0.000*** | 4.53 | 0.000*** | 2.72 | 0.007** | 4.35 | 0.000*** | 98.02 | 0.000*** |
| T0 - T3 | 0.74 | 0.025* | 3.88 | 0.000*** | 0.56 | 0.421 | 3.38 | 0.000*** | |||
| T2 - T3 | 4.44 | 0.000*** | 0.66 | 0.550 | 2.16 | 0.018* | 0.97 | 0.421 | 15.63 | 0.000*** | |
| Green 1: Active alert | T0 - T2 | 13.92 | 0.000*** | 15.06 | 0.000*** | 11.53 | 0.000*** | 12.41 | 0.000*** | 83.12 | 0.000*** |
| T0 - T3 | 7.39 | 0.012* | 11.56 | 0.000*** | 9.31 | 0.000*** | 8.790 | 0.002** | |||
| T2 - T3 | 6.53 | 0.070 | 3.50 | 0.194 | 2.22 | 0.468 | 3.62 | 0.208 | 6.65 | 0.010* | |
| Green 2: Passive alert | T0 - T2 | 15.65 | 0.000*** | 16.78 | 0.000*** | 24.13 | 0.000*** | 15.53 | 0.000*** | 159.69 | 0.000*** |
| T0 - T3 | 10.65 | 0.000*** | 13.94 | 0.000** | 7.19 | 0.017* | 14.26 | 0.000*** | |||
| T2 - T3 | 7.85 | 0.058 | 2.84 | 0.454 | 16.94 | 0.000*** | 1.26 | 0.773 | 12.49 | 0.000*** | |
| Amber: Inactive level | T0 - T2 | 17.47 | 0.000*** | 24.72 | 0.000*** | 19.13 | 0.000*** | 17.85 | 0.000*** | 94.21 | 0.000*** |
| T0 - T3 | 12.52 | 0.003** | 18.72 | 0.000*** | 5.34 | 0.251 | 15.44 | 0.000*** | |||
| T2 - T3 | 4.95 | 0.131 | 6.00 | 0.075 | 13.78 | 0.000*** | 2.41 | 0.512 | 15.25 | 0.000*** | |
| Red: Sleepy level | T0 - T2 | 14.95 | 0.000*** | 7.75 | 0.015* | 16.53 | 0.000*** | 10.09 | 0.000*** | 54.50 | 0.000*** |
| T0 - T3 | 5.52 | 0.151 | 6.78 | 0.024* | 11.16 | 0.006** | 7.62 | 0.027* | |||
| T2 - T3 | 9.44 | 0.003* | 0.97 | 0.547 | 5.38 | 0.072 | 2.47 | 0.364 | 11.44 | 0.001** | |
*p<0.05, **<0.01, ***<0.001 MSE=Multisensory Environment, MT=Massage Therapy, MT-MSE=Massage Therapy in Multisensory Environment, CB=Challenging Behaviour, MD=Mean Difference, p=significance level
Table 5: Comparison of mean scores of outcome measures within group across three measurement times (baseline and two posttests).
▪ Summary of the results
Interaction effect (time x group) was found in respiration rate, number of maladaptive behaviour, number and duration of adaptive behaviour. Group effect was shown in respiration rate, duration of adaptive behaviour, and sleepy state of AOC.
Respiration rate
The participants of MT-MSE group possessed the lowest respiration rate in T2 (mean value=15.72), but it changed to MSE group in T3 (mean value=15.77). The participants of control group maintained the highest respiration rates throughout the study (mean values>19). According to the hypothesis, it was perceived that lower respiration rate than baseline level indicated lower physiological arousal or activation of parasympathetic system, which implied a state of relaxation or low level of anxiety. From the results of respiration rate, all treatment groups had lower respiration rate than control group, in which, MSE was better than MT and MT-MSE at the end of the study period (T3).
Number of maladaptive behaviour
The results showed that the number of maladaptive behaviour of three treatment groups was higher than the control group (mean value=2.91) at T3, but not statistically significant. In fact, the participants of MT group exhibited the lowest maladaptive behaviour (mean value=2.19) among study groups at T2, and significantly lower than MT-MSE (mean value=4.97). MT group was recognized as partially supported the therapeutic effect on reducing the maladaptive behaviour than other treatment groups atablet T2 time-point only.
Number and duration of adaptive behaviour
The MT group obtained the highest number and longest duration of adaptive behaviour than the other three study groups at T2 and T3, in which, only mean values at T3 was significant different from MSE and MT-MSE. There was no significant difference between MT and control group. The therapeutic value of MT on adaptive behaviour was supported but the participants of control group had higher number and duration of adaptive behaviour than MSE and MT-MSE.
Sleepy state in alertness level
The MT group showed lowest sleepy state than other three groups at T2 (around 4%) and T3 (around 6%), in which, only result of T3 was significantly different from MSE (around 26%) and MT-MSE (around 18%). It seemed that participants of MT group were less sleepy during interventions, and such effect could substantiate after two weeks. By contrast, the participants of MSE and MT-MSE groups showed higher sleepy state than other groups at T3.
According to the overall percentage distribution of AOC, the dominant alertness levels in baseline assessment were inactive (maximum 67% in MT group) and sleepy states (maximum 55% in MSE group). It changed to passive alertness state (maximum 59% in MT-MSE group) at T2, and the major alertness states were shared between passive alertness (maximum 39% in MT group) and inactive state (37% in MT-MSE group) at T3.
It was hypothesized that active state would be the major alertness state after intervention given, it was partially supported in the study process because passive alertness is part of the active alert levels. According to the results, passive alertness was prominent at T2 and partially substantiated at T3 with group changed from MT-MSE to MT. The prevalence of passive alertness state over active alertness may be due to the physical disablement of the participants and the use of adaptive support; hence motionlessness was common, but maintained social contact with immediate environment. Generally, MT group was better than other treatment groups because the participants were not engaged in sleepy state.
Time effect
Time effect was prevalent in the study, except the pulse rate, number and duration of maladaptive behaviour which did not detect significant change in any study groups. The mean scores of all study groups were relatively stable between T2-T3 when compared with T0-T3; hence, variation between T2-T3 with significance level was limited. Most often, change patterns existed between T0-T2 and T0-T3 in the outcome measures. The primary outcome, i.e., frequency and severity of challenging behaviour, only showed significant change within group. The mean scores of both frequency and severity of challenging behaviour were decreasing in all study groups, but MSE group showed consistently different between T0- T2 and T0-T3 which did not find in other study groups.
The hypothesis of combined MT-MSE intervention that would have significantly decreased maladaptive behaviours and increased alert state (i.e., showing awareness to immediate environment) than the two single modes of intervention (MT or MSE alone) was not supported in the findings.
Discussion
According to the aim of the study, it was found that individual interventions had significant effect on particular outcome measures. For instance, participants of both MSE and MT-MSE groups obtained relatively lower respiration rate than the other two groups, indicating that they were in a state of parasympathetic activity which is comparable to relaxation effect. Such lower respiration rate was able to substantiate to 2-week follow up study. They were less sleepy during the interventions, but had significantly increased sleepiness after the cessation of interventions.
The increased sleepiness of MSE and MT-MSE after the interventions might be explained by the findings of Munde and her colleagues [25,28]. They had similar findings in the observations of MSE activity. They explained that persons with SPID had poor perceptual capacity and low information processing that markedly reduced subject’s attention span. The sensory stimulations of MSE quickly made persons with SPID exhausted after repeated exposure of sensory stimulations. The alertness level was substantially decreased but rapidly shifted between different alertness levels. Such rapid shifting between alertness levels was described as “waves”, which might not be instantly picked up by the on-site observer [25,28]. Hence, it would be considered shortening the observation interval to less than 20 seconds and use of video-taking to capture the rapid shifting of different alertness levels in the future studies.
Regarding the substantive effect of intervention groups, the participants of massage therapy exhibited significant higher number and duration of adaptive behaviour than other study groups, as well as less sleepy than other study groups. Such phenomenon was able to substantiate over to the usual care environment. Literature of massage therapy [9,29] revealed that increased positive behaviours which referred to communication intention, relationship building, engagement behaviour, social awareness, and concentration span [3] were increased following massage therapy. Though the concentration span of residents with SPID was short, the nature of activity was far more important than their diagnosis per se [29]. Massage therapy provided a non-threatening communication and emotional bonding between the therapist and the resident [8,9]. Subsequently, the duration of physical engagement and attention increased; hence the carryover effect to the usual care was sustained.
In correspondence to the objectives of the study, the intervention groups, i.e. MSE, MT, and MT-MSE were more effectiveness to induce relaxation, and adaptive behaviour than the control group, except reduction of maladaptive behaviour. Though the mean differences of control group between MSE and MT-MSE, were not significant, the sudden drop of maladaptive behaviour during non-interventional period from week 11 to 12 in control group was hard to explain.
▪ Passive recipients
The prevalence of time effect within group indicated that the participants with SPID were easily affected by different interventions, including social interaction and attention in the control group, as they were usually described as passive recipients because of their complex disabilities [30], even multisensory environment also promoted passivity of the participants [7,31]. Strategies to engage in adaptive behaviours and reduce challenging behaviours are the major concern in the field of ID. Positive interventions are more effective than aversive methods, especially for sensory-reinforced challenging behaviours [32,33]. Apart from MSE, massage therapy offers tactile sensation for active engagement and physical proximity [8], especially for those with visual and/or hearing impairments.
▪ Substantiation of treatment effects
As the data profile BPI-01 was a behavioural summary of the past two weeks in usual care environment and the other outcome measures were obtained during or just after the intervention session, the social atmosphere and other residents’ behaviours in the usual care have overwhelmed to the therapeutic effect of the interventions which considered short-lived and prone to vanish if adverse physical environment existed [34].
Corresponding to the conceptual framework of challenging behaviour [34], the adoption of positive behaviour support (PBS) in service system is postulated because it emphasizes the proactive strategies to relieve the vulnerabilities of individual SPID residents, for instance, medical treatment for treating the underlying physical illness and pain which would affect the appreciation of leisure activity, provisions of enriched environment, and active engagement of meaningful activity.
▪ Cost-effectiveness Analysis of the Interventions
In view of different interventions in the study, MSE requires the most expensive equipment and intervention than others in terms of hardware installation and maintenance disregard the expenditure of manpower resources. However, the therapeutic value of MSE intervention was not significant or outstanding. Generally, massage therapy appeared superior to other interventions, in consideration of adaptive behaviour and alertness level.
From the results of the study, the generalized improvement of outcome measures within individual groups implied that the therapeutic value of social interaction and attention might be considered as one of the interventions and worth to verify in the future studies in respect to the evaluation of cost-effectiveness of different interventions.
Limitations of the Study
• The number of participants should be increased to enhance the statistical power.
• In view of rapid shifting of alertness states, short observation interval should be considered to increase the accuracy to capture the alertness changes. Video-taking may be considered, so that it could be viewed repeatedly to assure the precision of outcome measures.
• The intensity of treatment sessions in terms of dose and duration should be enhanced, for instance, increased the frequency of the interventions from twice per week to three times a week.
• The selection of outcome measures should be more precise to identify behavioural changes. For instance, the observation of Behaviour Problems Inventory (BPI-01) is reduced to previous one week in the usual care instead of two weeks to enhance the accuracy of the rating.
• Since one of the selection criteria was to exclude those restless residents who often exhibit severe challenging behaviours, hence the degree of behavioural changes between pre- and post-interventions may be restricted.
Implications for Future Studies
Despite sensory deficits would affect the appreciation of MSE and MT-MSE, it is difficult to exclude residents with visual and hearing impairment in the study, because the prevalence of sensory defects is high in persons with SPID. A study showed more than 50% of people with profound ID having visual impairment [35]. If these subjects were excluded, the sample size and statistical power would be tremendously upset. Interventions that would not affect the enjoyment of activity for persons with sensory deficits may consider in future studies e.g., aromatherapy, sensory garden, and air bouncer.
Nevertheless, some therapeutic effects of MT-MSE were noted in respiration rate and passive alertness state after 5 weeks of intervention. In light of sensory exhaustion from repeated exposure, the duration of MT-MSE interventions can be considered to shorten to 5 weeks or less in future studies, given that its cost-effectiveness and therapeutic value.
Conclusion
In long-term care setting, the hours of residents staying in usual care environment are often more than participation of structured activity; hence a therapeutic milieu in the living environment is vital to control the exhibition of challenging behaviour. To prolong the therapeutic values of meaningful activity, like massage therapy and multisensory environment, the adoption of positive behaviour support in the service system is suggested for longer term effect in managing challenging behaviour.
Acknowledgments
We would like to thank all participants, and involved carers for their contributions and logistic supports throughout the study period.
Conflict of interest
The authors declared no conflict of interest.
Clinical trials registration number (identifier)
ClinicalTrials.gov; Registration No.: NCT02120820
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (5th edt.) – DSM-5(TM). Arlington, VA: American Psychiatric Publishing, 2013.
- Secretary for Labour and Welfare Bureau. Hong Kong: The facts – Rehabilitation. Hong Kong, Information Services Department, 2015.
- Chan SWC, Thompson DR, Chau JPC, et al. The effects of multisensory therapy on behaviour of adult residents with developmental disabilities – A systematic review. Int. J. Nurs. Stud 47(1), 108-122 (2010).
- Emerson E. Challenging Behaviour - Analysis and Intervention in People with Severe Intellectual Disabilities, Cambridge. Cambridge University Press, 2001.
- Emerson E, Robertson J, Gregory N, et al. Treatment and management of challenging behaviours in residential settings. Journal of Applied Research in Intellectual Disabilities 13 (4), 197-215 (2000).
- Emerson E. Challenging Behaviour - Analysis and Intervention in People with Severe Intellectual Disabilities, Cambridge: Cambridge University Press, 2001.
- Vlaskamp C, de Geeter KI, Huijsmans LM, et al. Passive activities - The effectiveness of multisensory environments on the level of activity of individuals with profound multiple disabilities. J. Appl. Res. Intellect. Disabil 16, 135-143 (2003).
- Ayer S. Use of multi-sensory rooms for children with profound and multiple learning disabilities. Journal of Learning Disabilities for Nursing, Health and Social Care 2(2), 89-97 (1998).
- Solomons S. Using aromatherapy massage to increase shared attention behaviours in children with autistic spectrum disorders and severe learning difficulties. British Journal of Special Education 32(3), 127-137 (2005).
- Lindsay WR, Pitcaithly D, Geelen N, et al. A comparison of the effects of four therapy procedures on concentration and responsiveness in people with profound learning disabilities. J. Intell. Disabil. Res 41, 201-207 (1997).
- Lindsay WR, Black E, Broxholme S, et al. Effects of four therapy procedures on communication in people with profound intellectual disabilities. J. Appl. Res. Intellect. Disabil 14(2), 110-119 (2001).
- Gescheider GA, Bolanowski SJ, Hall KL, et al. The effects of aging on information-processing channels in the sense of touch: I. absolute sensitivity. Somatosens. Mot. Res 11(4), 345-357 (1994).
- Humes LE, Busey TA, Craig JC, et al. The effects of age on sensory thresholds and temporal gap detection in hearing, vision, and touch. Atten. Percept. Psychophys 71(4), 860-871 (2009).
- Portney LG, Watkins MP. Foundations of clinical research: application to practice (3rd edt.). New Jersey: Pearson Prentice Hall, 2009.
- Chan SWC, Chien WT, To MYF. An evaluation of the clinical effectiveness of a multisensory therapy on individuals with learning disability. Hong. Kong. Med. J 13(1), 28-31 (2007).
- Martin NT, Gaffan EA, Williams T. Behavioural effects of long-term multi-sensory stimulation. Br. J. Clin. Psychol 37(1), 69-82 (1998).
- Moyer CA, Rounds J, Hannum JW. A meta-analysis of massage therapy research. Psychol. Bull 130(1), 3-18 (2004).
- Montori VM, Guyatt GH. Intention-to-treat principle. CMAJ 165(10), 1339-1341 (2001).
- Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. J Pharmacol Pharmacother 1, 100-107 (2010).
- Lotan M, Gold C. Meta-analysis of the effectiveness of individual intervention in the controlled multisensory environment (Snoezelen) for individuals with intellectual disability. J. Intellect. Dev. Disabil 34(3), 207-215 (2009).
- Moraska A, Pollini RA, Boulanger K, et al. Physiological adjustments to stress measures following massage therapy: A review of the literature. Evid. Based. Complement. Alternat. Med 7(4), 409-418 (2008).
- Sanderson H, Harrison J, Price S. Aromatherapy and Massage for People with Learning Difficulties. Birmingham: Hands On Publishing. 1991.
- Rojahn J, Matson JL, Lott D, et al. The behaviour problems inventory: An instrument for the assessment of self-injury, stereotyped behaviour, and aggression / destruction in individuals with developmental disabilities. J. Autism. Dev. Disord 31(6), 577-588 (2001).
- Vlaskamp C, Fonteine H, Tadema A, et al. Manual for the “alertness in people with profound intellectual and multiple disabilities” checklist. Netherlands: Stichting Kinderstudies, 2009.
- Munde VS, Vlaskamp C, Maes B, et al. Catch the wave! Time-window sequential analysis of alertness stimulation in individuals with profound intellectual and multiple disabilities. Child. Care. Health. Dev 40(1), 95-105 (2012).
- Shapiro M, Parush S, Green M, et al. The efficacy of the ‘Snoezelen’ in the management of children with mental retardation who exhibit maladaptive behaviours. British Journal of Developmental Disability 43(2), 140-155 (1997).
- Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics 42, 121-130 (1986).
- Munde VS, Vlaskamp C, Ruijssenaars AJJM, et al. Determining alertness in individuals with profound intellectual and multiple disabilities: the reliability of an observation list. Educ .Train. Autism. Dev. Disabil 46(1), 116-123 (2011).
- McEvoy, C., Perrault, A., & Graetz, J. The use of massage therapy in the treatment of self-injurious behavior. Wayne County Intermediate School District. Unpublished manuscript, 1987.
- Munde V, Vlaskamp C. Initiation of activities and alertness in individual with profound intellectual and multiple disabilities. J. Intellect. Disabil. Res 59(3), 284-292 (2015).
- Munde VS, Vlaskamp CV, Ruijssenaars AJJM, et al. Alertness in individuals with profound intellectual and multiple disabilities: A literature review. Res. Dev. Disabil 30, 462-480 (2009).
- Case-Holden V, Hupp SC. Reducing stereotypic handmouthing of a child with severe/profound retardation. J. Early. Interv 13(2), 165-172 (1989).
- Lanovaz MJ, Robertson KM, Soerono K, et al. Effects of reducing stereotypy on other behaviors: A systematic review. Res. Autism. Spectr. Disord 7(10), 1234-1243 (2013).
- Hastings RP, Allen D, Baker P, et al. A conceptual framework for understanding why challenging behaviours occur in people with developmental disabilities. International Journal of Positive Behavioural Support 3(2), 5-13 (2013).
- Evenhuis HM, Theunissen M, Denkers I, et al. (2001) Prevalence of visual and hearing impairment in a Dutch institutionalized population with intellectual disability. J. Intellect. Disabil. Res 45, 457-464 (2001).