Research Article - (2018) Volume 8, Issue 4
A Case of Right Frontal Lobe Dysfunction with Risk Behaviors, Despite Normal General and Risk Cognition: Misunderstood as Cheerful, Active, and Careless Character?
- Corresponding Author:
- Kenichi Meguro, MD
Geriatric Behavioral Neurology, Tohoku University CYRIC, 4-1, Seiryo-machi, Aobaku, IDAC, 980-8575 Sendai, Japan
Tel: 81 22 717 7359
Abstract
Some older community residents can exhibit baffling behaviors in daily life, despite their memory and general cognitive functions being normal. Thus, they may be superficially suspected to have a psychiatric disease. We experienced a case in which risk behaviors related to fire, consumer damage, fall, etc. and hyperactivity were observed in daily life; despite general cognitive function being within a normal range. Her abnormal behaviors were summarized by behavioral neurology, as follows: 1) hyperactivity caused by right hemisphere damage, 2) decreased right frontal lobe function caused by right frontal lobe damage, and 3) confabulation caused by disinhibition of the left frontal lobe. Thus, we performed neuroimaging examinations, and found right basal ganglia infarction (MRI) and decreased blood flow to the right frontal lobe (single photon emission computed tomography [SPECT], remote effect). After a service representatives meeting, where the physician in charge provided an explanation, the patient, who did not like drug administration by nature, and had thus refused recommendations from her home doctor, began to be conscious about her disease and agreed to undergo drug treatment. It is not easy to explain the relationship between cerebral infarction in a strategically important region and daily life (behavior). This is the specialty of dementia medicine. When a disease is found to exhibit cerebral injury, the patient will be able to correctly understand the disease, and appropriate care will be promoted under the health management and collaboration between medical and nursing care.
Keywords
Frontal lobe, Hyperactivity, Confabulation, Vascular dementia, Cerebral infarction
Background
Since Alzheimer disease (AD), a representative underlying disease of dementia, begins with amnesia, followed by delusion of theft [1] and other behavioral disorders, family and local residents can become aware of the disease. Thus, treatment by a specialist may be easily provided to such cases; although some cases may be misunderstood as aging phenomenon. Hippocampal atrophy and decreased cerebral blood flow in the frontal/parietal lobes [2,3] are easily understood as the neural basis of amnesia and other symptoms, and can easily be explained as the reason for diagnosis, oral administration of donepezil, etc. , and the commencement of psychosocial intervention [4] to the patient and care providers.
However, another underlying disease, vascular dementia [5] or vascular cognitive impairment [6], is not quite as simple as AD. Cerebrovascular disorder exhibits different symptoms, depending on the site of the damage, on the right or left, and in case of a lesion in the left hemisphere, aphasia and motor paresis of the dominant hand are easily observed. However, in case of a lesion in the right hemisphere, the disease can be difficult to find, due to the anosognosia [7] which is associated with many cases. In addition, since memory is relatively maintained in such cases, it is difficult to consider that such changes in behaviors were caused by cerebral injury. When awareness of the disease is low, it is difficult to identify such cases to then provide treatment by a specialist.
Some older community residents exhibit baffling behaviors in daily life, despite maintaining normal memory and general cognitive functions, and thus, they may be superficially suspected as having a psychiatric disease. We experienced a case in which risk behaviors related to fire, consumer damage, fall, etc. and hyperactivity were observed in daily life, despite the fact that the general cognitive function was within the normal range at our dementia specialty outpatient clinic. This case was considered to be caused by the effects of right hemisphere damage. Based on this case, we discussed the importance of early imaging diagnosis and collaboration between medical and nursing care for older community residents with problems in daily risk management.
Ethical Consideration
We obtained written informed consent from the patient and her family for publication of the report. Careful attention was paid to protect personal information and confidentiality.
▪ Case: A 72-year-old right-handed woman chief complaint
Patient: Amnesia (memory loss related to an object)
Family: Abnormal risk management behaviors (accidental fire, consumer damage, and hyperactivity), and abnormal domestic behaviors (egestion and the act of eating)
▪ Life history
In 1943, the patient was born as the second daughter, with 2 brothers/sisters, of parents who operated a shop (stationary and foods). Due to an accident at birth, she had a visual disturbance in her left eye.
After graduating from a junior college of nurtures (schooling history: 14 years), she married and had 3 children. Even after childbirth, she continued working as a nurse, devoting her life to the work. She was not good at housekeeping, since the days when she worked as a nurse.
Even after retiring as the head of a nursery school at the age of 60 years, she has been involved in local childcare at her home with her husband. She has been a sociable person, and lived an active life by participating in local volunteer activities, hobbies, lifelong learning, etc.
▪ Family history
No special notes
▪ Past medical history
Depression with no detailed information and left varicose vein in her 50s Mild diabetes mellitus and hypertension since the age of 62 and 71 years, respectively.
▪ History of present illness
She had amnesia after retiring at the age of 60, but details regarding the time could not be identified. In addition, reduced level of housekeeping (difficulty in cooking and clearing up), and hyperactivity (excessive dependence on regional social activities with no plan) were observed. She exhibited casual characteristics when she began to operate an unauthorized childcare facility for local children with no idea about the preparation of lunch.
These symptoms became aggravated after her husband died, when she was 68 years old. The number of accidents, i.e., burning of a pan, purchase of expensive products, i.e., a feather quilt, health appliances (600,000-yen magnetic necklace), water purifier (480,000 yen), underwear, etc., fall, and injury, increased. In addition, she also exhibited abnormal behaviors in daily life, such as evacuation using a bucket in a kitchen and sites other than the toilet, and eating by catching food by hand.
One summer, when she was 71 years old, she burned deadwood in an incinerator on her property, causing a fire spread to the surrounding bank and mountain forest.
In July, when she was 72 years old, she became aware of the fact that she stumbled over a step because she could not raise her lower extremities, due to left lower extremity pain during walking. She called the Community General Support Center to consult about a house renovation using the Long-term Care Insurance. When a member of the Community General Support Center visited her house, various items were scattered about the house. In addition, she had the burden of spending time looking for an item that she had misplaced or did not put back, and she recognized her memory loss. When she applied for nursing care insurance, she was certified as requiring support level 1.
In September when she was 72 years old, cleaning support was introduced for 1 hour twice a week, as home-visit nursing care of the nursing care insurance service, but she frequently forgot and went out on the day of the service. Her amnesia, reduced level of housekeeping, risk behavior, abnormal behavior, and hyperactivity were gradually aggravated.
She complied with the recommendation that had been made continuously by her family, and consulted with the regional inclusive support center about her severe amnesia. After referral to visit a specialist, she visited our dementia specialty outpatient clinic with her eldest daughter in November, when she was 72 years old.
▪ Present illness
Test findings at general internal medicine: Blood pressure 148/91 mmHg, HbA1c 6.5 (normal range: 4.6 - 6.2)
▪ Neurological findings
Visual impairment of the left eye and decreased sensation on the left side of the body
▪ Neurobehavioral findings
General cognitive function, a high mini mental state examination (MMSE) [8] total score of 26, suspected confabulation based on her talkativeness during the interview.
Based on these findings, we performed detailed neuropsychological tests, suspecting the following, because she exhibited decreased sensation on the left side of the body, despite preservation of general cognitive function:
1. Hyperactivity caused by right hemisphere damage
2. Decreased right frontal lobe function caused by right frontal lobe damage
3. Confabulation caused by disinhibition of the left frontal lobe
▪ Neuropsychological findings
Table 1 presents the points of memory, language, visuospatial function, and judgment.
| Examinations | Assessments | |
|---|---|---|
| Memory | episodic memory,WMS-R(memory) | 〇 |
| Language | naming, repetition, auditory comprehension, writing | 〇 |
| confabulation | ++ | |
| copying | 〇 | |
| Visuospatial function | The Baum Test (free drawing) | △ |
| Visual description test (hazard anticipation) | 〇 | |
| coping behavior for consumer damage | 〇 | |
| Judgment | ||
| Picture Arrangement Test | △ |
Table 1: Neuropsychological findings.
▪ Confabulation test
In the Dara Barba confabulation test [9], both episodic confabulation [10-12], in which a patient talks about a fictional event as if it actually happened, and semantic confabulation [10-12], in which a patient talks continuously about knowledge that the patient never had. The following is part of the question and answer in the interview to our patient.
Q.: Do you remember what you had as dinner on November 3, 1991? (Correct answer: “No idea”)
A.: 25 years ago…. I show an outline. It should be Culture Day Holiday. I had some sake. Then, a cup of soup, clear soup, like that… and rice boiled with red beans, something like that, to celebrate the day. For dinner, such rice with dishes of fish, vegetables, cabbage, onion, salad-like vinegar dish, and sweet bean jelly or Manju as a dessert.
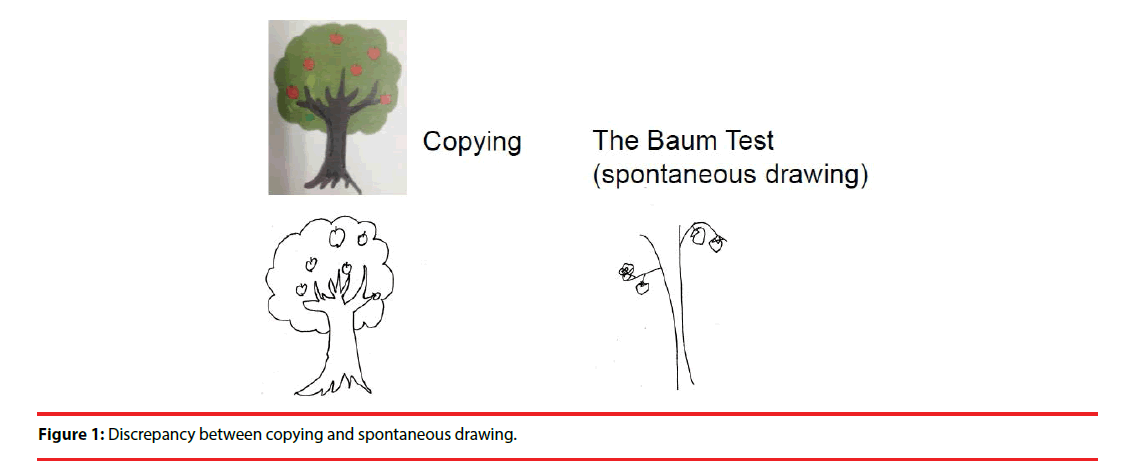
▪ Copy of a picture and spontaneous drawing
Although she could copy a picture, her spontaneous drawing was poor, suggesting expression impairment (Figure 1). She was asked to copy a model picture of “a tree with apples.” For free drawing, we asked her to “draw a picture of a tree with fruit” (Baum Test) [13], so that she would draw a picture freely on a piece of A4 paper.
▪ Visual description test and judgement test
The results of a “hazard anticipation questions with scene images” [14], which was performed because she exhibited risk behaviors, were favorable, and she completely understood coping behavior for consumer damage and quotation.
However, the results of the “Picture Arrangement Test [15],” in which the patient is asked to appropriately line up multiple pictures in chronological order, were poor, suggesting a suspected decrease in future forecast.
▪ Assumed relationship with cerebral functions
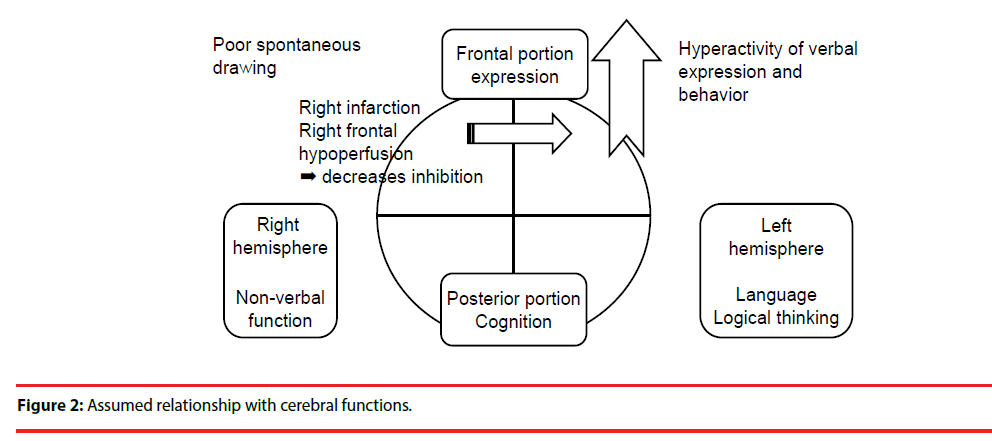
The relationship with cerebral functions based on the behaviors and psychological findings of Ms. Y is shown in Figure 2.
The frontal portion of the brain is responsible for expression and motion, while the posterior portion is responsible for cognition and memory. The left hemisphere is responsible for language and mathematical computation, while the right hemisphere is responsible for visuospatial recognition and nonverbal function.
Cognition in Ms. Y was preserved, showing that posterior brain function was maintained, but it was assumed that the difference between the right and left hemispheres would be large in the frontal portion. Since the right and left hemispheres inhibit individual actions reciprocally, in order to maintain good balance, it was assumed that disinhibition of the left hemisphere was caused by damage to the right hemisphere in the patient, because she exhibited confabulation, talkativeness, hyperactivity, consumer damage induced by talking, etc.
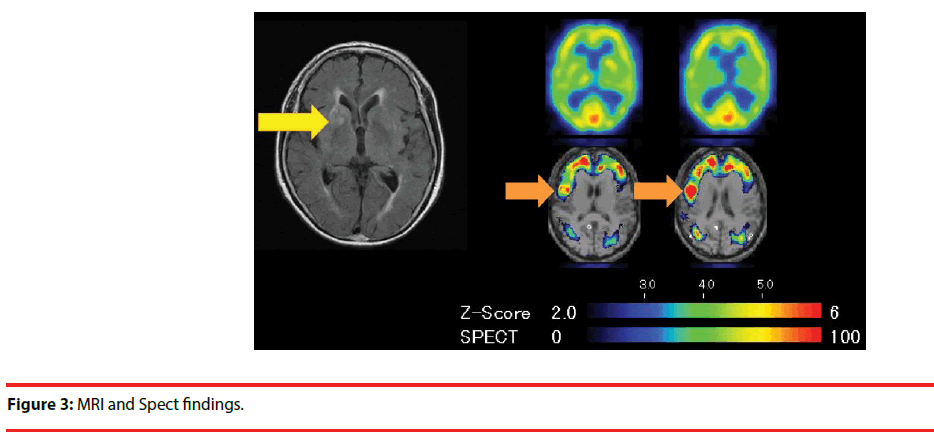
Neuroimaging findings MRI: Right basal ganglia infarction (Figure 3)
SPECT: Decreased blood flow in the right frontal lobe (remote effect).
We used an eZIS system [16] based on the same idea of SPM (eZIS is an automatic and Matlab® free version of SPM). Using voxel-based spatial normalization, a SPECT image of one subject was converted into the same stereotaxic space as normal age-matched database images. Voxelwise z-score [{(CBF of patient)-(CBF of normal database)}/ (SR)] were computed, and voxels having supra threshold (p<0.05) were detected as significant areas
▪ Diagnosis
Vascular dementia (right basal ganglia infarction)
▪ Medical and nursing care collaboration and successive processes
After the diagnosis was made, a policy-making meeting (service representatives meeting) was held with the participation of the patient, her eldest daughter, a nurse from the regional inclusive support center who also worked as a nursing care support specialist, and the physician in charge. The physician explained the necessity of drug treatment to prevent redevelopment of the cerebral infarction by presenting imaging test results. Based on the fact that she lived alone in the daytime and understood the needs for support, it was determined that a drug treatment support system would be prepared for the patient.
Although the patient forgot about housing of a thing and had a certain level of memory disturbance with respect to a schedule, etc., she remembered the details of the explanation about her disease conditions and improvement of daily life provided by the physician, 2 weeks after the explanation. She originally did not like drug treatment, and thus did not follow the recommendations of her home doctor. However, she responded differently this time, and began to be conscious about her disease. After obtaining an active agreement for drug treatment from the patient, drug treatment was commenced.
Her second son who lived with the patient described that the patient had a strong recognition of drug treatment, for example, she kept the drug in the same place, and left the empty drug package after taking the drug so that he could confirm the administration. Ms. Y said, “Reassurance is most important for me. Drug intake is not hard for me. It is my job.”
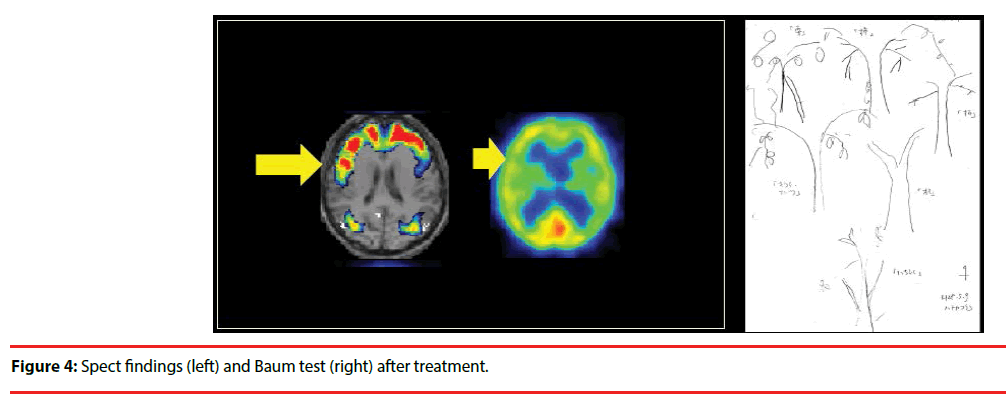
One month after commencement of drug treatment, her behaviors and the results of the Baum Test were improved; although no change was observed in the MMSE (27 points) (Figure 4). In the second image diagnosis, improvement was confirmed in blood flow of the right frontal lobe.
Discussion
Although there was the possibility that the patient might be overlooked because her general cognitive function was normal and memory level was favorable, the difference between various positive findings (talkativeness, hyperactivity, and confabulation)/risk behavior and cognitive function could be understood based on cerebral injury.
Although her family initially felt confused because they could not understand whether the patient was normal or had a disease, they were able to fully understand the medical findings that showed the development of cerebral injury. Local residents might overlook the disease because they thought the patient exhibited “positive, active, and careless characteristics.”
When her disease was clarified as cerebral injury being responsible for her behaviors, the patient became conscious about her disease, and was able to voluntarily begin the treatment. As a result, her symptoms and life habits improved. When considering the ability to take drugs from a behavioral neurological standpoint, the process of drug intake action includes: 1) understanding of the disease (semantic memory), 2) understanding of the drug (semantic memory), and 3) drug intake action as a function to be performed. It was estimated that Ms. Y, who was able to maintain memory despite the chief complaint of amnesia, could become conscious about the disease after receiving an explanation from a specialist, and began to receive treatment for the dementia under agreement.
The fact that the service representatives meeting was held cooperatively by a variety of concerned persons, including the patient as the main person, might have had a large impact on the memory of Ms. Y. However, since human resources are insufficient in actual medical nursing care practice, opportunities for collaboration (cooperative work) should be ensured not only for the commencement of treatment, but also in holding face-to-face meetings of service representatives, by determining the compensations for both outpatient clinics of medical institutions and nursing care support offices.
It can be expected that the patient’s family will be able to more correctly understand the situation of the patient, and reduce the nursing care burden by using health management and nursing care services under collaboration between medical and nursing care, and to ensure the promotion of appropriate nursing care, including risk management.
However, it remains difficult to explain the relationship between the infarction in the strategic area [17] and daily life (behavior). This is the specialty of dementia medicine. When it is clarified that the disease is due to cerebral injury, the patient will be able to understand the disease correctly, and health management and appropriate care will be promoted through collaboration between medical and nursing care. We plan to perform further investigations with more subjects in the future.
References
- Nakatsuka M, Meguro K, Tsuboi H, et al. Contents of delusional thoughts in Alzheimer’s disease and content-specific brain dysfunction assessed with BEHAVE-AD-FW and SPECT. International. Psychogeriatrics 25(6), 939-948 (2013).
- Yamaguchi S, Meguro K, Itoh M, et al. Decreased cortical glucose metabolism correlated with hippocampal atrophy in Alzheimer’s disease as shown by MRI and PET. J. Neurol. Neurosurg. Psychiatry 62(1), 596-600 (1997).
- Meguro K, LeMestric C, Landeau B, et al. Relations between hypometabolism in the posterior association neocortex and hippocampal atrophy in Alzheimer’s disease: A PET/MRI correlative study. J. Neurol Neurosurg. Psychiatry 71(1), 315-321 (2001).
- Meguro K. Cholinesterase inhibitors are compatible with psychosocial intervention for Alzheimer disease patients suggested by neuroimaging findings. Psychiatry. Res. Neuroimaging 259(1), 29-33 (2017).
- Nakatsuka M, Meguro K. Neuroepidemiology of vascular dementia. Vascular.Dementia:. Risk Factors, Diagnosis. and .Treatment. Nova Publishers, (2011)[E-book].
- Ishii H, Meguro K, Yamaguchi S, et al. Prevalence and cognitive performances of vascular cognitive impairment no dementia in Japan: the Osaki-Tajiri Project. Eur. J. Neurol 14(1), 609-616 (2007).
- Tezuka K, Meguro K, Akanuma K, et al. Overestimation of self-reported ADL in vascular dementia patients with a right hemisphere lesion. J. Stroke. Cerebrovascular. Dis 22(1), 9-14 (2013).
- Folstein FM, Folstein SE, McHugh PR. ‘‘Mini-mental state’’ a practical method for grading the cognitive state of patients for the clinician. Journal.of .Psychiatry. Res 12(1), 189-198 (1975).
- Dalla Barba G, Nedjam Z, Dubois B. Confabulation, executive functions, and source memory in Alzheimer’s disease. Cogn. Neuropsychol 16(1), 385-398 (1999).
- Lee E, Meguro K, Hashimoto R, et al.Confabulations in Episodic Memory are Associated with Delusions in Alzheimer’s disease. J. Geriatr. Psychiatr. Neurol 20(1), 34-40 (2007).
- Lee E, Akanuma K, Meguro M, Ishii H, Yamaguchi S, Meguro K. Confabulations in remembering past and planning future are associated with psychiatric symptoms in Alzheimer’s disease. Arch. Clin. Neuropsychol 22(1), 949-956 (2007).
- Lee E, Kinomura S, Meguro K, et al. Confabulations on episodic and semantic memory questions are associatedwith different neurological backgrounds in Alzheimer’as disease. Cogn.Behav. Neurol 22(1), 81-88 (2009).
- Koch K. Der Baumtest. Der Baumzeichenversuch als psichodiagnostichesHilfsmittel. Verlag Hans Huber, Bern, Switzerland, 1949, K. Koch, Il reattivodell’albero. Il disegno dell’albero come ausilio psicodiagnostico. Giunti O.S.Organizzazioni Speciali, Firenze, Italy, (Italian edition), (2007).
- Akanuma K, Nakamura K, Meguro K, et al. Tome Project Members. Disturbed social recognition and impaired risk judgement in older residents with mild cognitive impairment after the Great East Japan Earthquake of 2011: the Tome Project. Psychogeriatrics 16(6), 349-354 (2016).
- Kato Y, Meguro K, Nakatsuka M, et al. Impaired Picture Arrangement subscores (WAIS-III) associated with decreased place orientation and frontal/occipital blood flow in Alzheimer’s disease: Implications for social judgment dysfunction. The Osaki-Tajiri Project. Psychiatry Res. Neuroimag 256(1), 65-69 (2016).
- Kanetaka H, Matsuda H, Asada T, et al. Effects of partial volume correction ondiscrimination between very mils Alzheimer’s disease and controls usingbrain perfusion SPECT. Eur. J. Nucl Med Mol Imaging 31(1), 975-980 (2004).
- Meguro K, Tanaka N, Nakatsuka M, et al. Vascular lesionsin mixed dementia, vascular dementia, and Alzheimer’s disease withcerebrovascular disease: The Kurihara Project. J. Neurological Sciences 322(1-2), 157-160 (2012).